 by Carolyn Thomas ♥ @HeartSisters
by Carolyn Thomas ♥ @HeartSisters
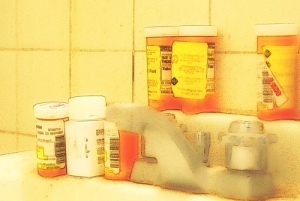
Anything you put into your mouth has an effect on your body, but ingesting a drug, either prescribed by your doctor or an over-the-counter (OTC) drug like simple headache pills from your local grocery store can be downright dangerous if you are not careful. Here are 10 common – and potentially fatal – medication errors, courtesy of Caring.com:
1. Confusing two medications with similar names – up to 25% of all reported errors are with meds that sound the same. Examples of commonly confused pairings include Adderall (a stimulant used for ADHD) versus Inderal (a beta-blocker used for high blood pressure).
2. Taking two or more drugs that magnify each others’ effects – be careful if you’ve been prescribed the blood-thinner Coumadin (warfarin), “the king of drug interactions”. You need just the right amount of Coumadin in your system for it to work properly; too much or too little and you could have serious heart problems such as arrhythmias or a stroke. Because so many other drugs interfere with its action, extreme caution is a must.
3. Overdosing by combining more than one medication with similar properties – you might have one medication prescribed to treat pain, another for anxiety, and another given as a sleeping pill, but they’re all sedatives, and the combined effect is toxic.
4. Getting the dosage wrong – all it takes is a misplaced decimal point and 1.0 mg becomes 10 mg, a tenfold dosing error that could cause a fatal overdose.
5. Mixing alcohol with medications – alcohol, combined with a long list of painkillers, sedatives, and other medications, can become a deadly poison. In fact, many experts now say you shouldn’t drink when on ANY medication without first checking with your doctor.
6. Double-dosing by taking a brand-name drug and the generic version at the same time – for example, a common generic diuretic is furosemide. The brand name is Lasix. A patient might have a bottle of furosemide and a bottle of Lasix and not know they’re the same thing. In essence, the patient is taking twice the dose.
7. Taking prescription drugs and over-the-counter or alternative medications without knowing how they interact – some of the most common OTC drugs can cause serious reactions. A top contender is medicine-chest staple Maalox for digestive upset. A new and very popular version, Maalox Total Relief, contains an ingredient called bismuth subsalicylate that can react dangerously with anti-clotting drugs, drugs for hypoglycemia, and anti-inflammatories, particularly ibuprofen and other nonsteroidal anti-inflammatories, or NSAIDs.
8. Not understanding interactions between medications and your diet – the most serious culprit in this situation is grapefruit juice, which has unique properties when it comes to inactivating or overactivating medications. Grapefruit juice inhibits a crucial enzyme that normally functions to break down and metabolize many drugs, such as anti-seizure drugs and statins used to lower cholesterol. The overloaded liver can’t metabolize the medication, resulting in an overdose, with potentially fatal consequences.
9. Failing to adjust medication dosages when a patient loses kidney or liver function – loss of liver or kidney function impairs your body’s ability to rid itself of toxins or foreign substances, so medications can build up in the body at higher dosages than intended.
10. Taking a medication that’s not safe for your age – as we age, our bodies process medications differently; check the Beers List website to check on drugs that should not be taken if you0111’re over age 65.

Excellent info – thanks so much. I really like your site, lots of useful info to browse here both for women with heart conditions plus those who know somebody with heart disease.
LikeLike
I could not have said it better myself.
Your site is one of my new favorite bookmarks.
Cheers!
LikeLike