by Carolyn Thomas ♥ @HeartSisters
 A new cardiac study out of Montréal tells us yet again what women heart patients have already known for years: women receive poorer care during a heart attack than our male counterparts do. Quelle surprise . . . But one specific finding caught my eye: one of the cardiac procedures that these researchers compared in this study was the use of the diagnostic electrocardiogram test (ECG or EKG) in male and female heart attack patients.(1)
A new cardiac study out of Montréal tells us yet again what women heart patients have already known for years: women receive poorer care during a heart attack than our male counterparts do. Quelle surprise . . . But one specific finding caught my eye: one of the cardiac procedures that these researchers compared in this study was the use of the diagnostic electrocardiogram test (ECG or EKG) in male and female heart attack patients.(1)
They found that women were less likely than men to receive an electrocardiogram within the recommended 10 minutes of arriving in hospital with suspected cardiac symptoms.
It turns out, however, that even when we do finally get hooked up to a 12-lead EKG in a hospital’s Emergency Department, the doctors there may not be able to correctly interpret the “significant EKG changes” that identify heart disease.
Previous research has reported a disturbing reality about diagnostic EKGs, which is the likelihood that high-risk EKG abnormalities may NOT be detected by physicians working in Emergency Medicine.
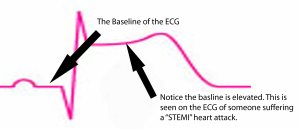 For example, a study published in the journal Circulation monitored five hospital Emergency Departments in California and Colorado over a two-year period to determine how often the treating Emergency physicians failed to identify “significant EKG changes” during a cardiac event.(2) The researchers concluded:
For example, a study published in the journal Circulation monitored five hospital Emergency Departments in California and Colorado over a two-year period to determine how often the treating Emergency physicians failed to identify “significant EKG changes” during a cardiac event.(2) The researchers concluded:
“Twelve per cent of patients studied had a high-risk EKG abnormality that was NOT detected by the Emergency Department provider. Rates of missed EKG findings from hospital to hospital ranged from 5.6% to 15.1%. Patients with missed EKG abnormalities tended to be older; more commonly had a history of heart failure or other cardiac history; and less frequently had chest pain as a presenting symptom”
That last factor is particularly disturbing, given that, depending on the study being cited, between 10% and 40% of women experience no chest pain during heart attack.(3)
Yet chest pain is still the primary cardiac red flag docs seem to be looking for. If chest pain is absent, are they then more likely to interpret EKG findings through the pre-judged lens of “not a cardiac event”?
In other words, if I show up to Emerg presenting with vague, atypical cardiac symptoms that many women experience during heart attack (like nausea, crushing exhaustion, shortness of breath or upper back/jaw pain) but no chest symptoms, I may face a greater risk of having my EKG misinterpreted compared to my male counterparts – even if it contains “significant high-risk EKG abnormalities”.
Here’s how that looks in real life. A reader named Lori described her own experience with “normal” EKG tests in her response to my post, How Does It Really Feel to Have a Heart Attack? She wrote:
“I know this from experience. A ‘normal’ EKG does not mean you don’t have heart problems. I had a heart attack at age 46. My main artery was 99% blocked. I now have two stents. My dad and my brother also had heart attacks at age 46. Their EKGs were always ‘normal’. My grandfather on my mom’s side died of a heart attack at 52. His EKGs were ‘normal’. My mom was short of breath and went to the doctor: her EKG was ‘normal’. She now has two stents. Please don’t let a doctor tell you that you don’t have heart problems just because your EKGs are ‘normal’.”
Also disturbing is the conclusion of the Circulation paper:
“The failure to identify high-risk findings was independently associated with a higher odds of not receiving ideal treatment.”
This makes perfect sense. Any physician who misinterprets “significant EKG changes” as being ‘normal’ is unlikely to recommend further appropriate cardiac treatment for the patient. Any diagnostic test is only as good as the interpretation of that test by the physician reading the test results.
Consider, for example, a study on the performance of radiologists done at Michigan State University by Dr. E. James Potchen.(4)
When radiologists were shown a chest x-ray of a patient with a missing clavicle (collarbone), 60% of them failed to identify the missing clavicle. And when this group of radiologists were shown a series of chest x-rays that included duplicate films, their interpretations disagreed among each other an average of 20% of the time. But even more interesting, when researchers showed them x-rays they had already interpreted, they disagreed with their own previous interpretations 10% of the time.
One of the most troubling aspects of Dr. Potchen’s study was the degree of certainty that the most accurate doctors had compared to the least accurate. For example, he compared the top 20 radiologists studied (95% diagnostic accuracy) with the bottom 20 (75% accuracy) and found that the specialists who performed poorly were not only inaccurate, they were also very confident that they were right when they were, in fact, quite wrong.
But how can this happen? How can trained, intelligent people with the letters M.D. after their names misinterpret diagnostic tests that clearly show abnormalities?
One theory behind such errors is what’s known as confirmation bias. (See also Experts: Why So Wrong So Often?)
Confirmation bias refers to a type of selective thinking in which we tend to notice and to look for what confirms our beliefs. Not only that, but we then want to ignore, or undervalue, or not even look for the relevance of anything that contradicts those beliefs.
For more on how doctors make critical thinking errors, consider what Dr. Pat Croskerry teaches about this subject. Dr. Croskerry is a trailblazer in teaching med students the skills of critical thinking. He implemented at Dalhousie University in Halifax the first undergraduate course in Canada teaching students about medical error in clinical decision-making, specifically around why and how physicians make diagnostic errors.
As a heart attack survivor who was misdiagnosed with acid reflux in the E.R. and sent home (despite presenting with textbook heart attack symptoms like debilitating central chest pain, nausea, sweating and pain radiating down my left arm), I’m no stranger to the damage caused by experts who are wrong.
My EKG that morning was ‘normal’.
My cardiac enzymes were ‘normal’.
My treadmill stress test was ‘normal’.
And I was home within five hours of the onset of my symptoms – far earlier than most cardiac treatment guidelines recommend in order to correctly identify myocardial infarction. As cardiologist and founder of the Mayo Women’s Heart Clinic Dr. Sharonne Hayes explained:
“Treatment guidelines help women get the care that has been shown to improve survival and long term outcomes in large groups of patients.
“Part of the problem now is that the guidelines are less likely to be applied to women compared to men. We know that when hospitals have systems in place to ensure they provide care according to the guidelines, women’s outcomes improve, even more than men’s.”
Women under the age of 55 are in fact seven times more likely than men are to be misdiagnosed in mid-heart attack and sent home.(4) About 5% of autopsies find clinically significant conditions that were missed and could have affected the patient’s survival. And over 40% of medical malpractice suits are for failure to diagnose. The good news, as Erin Anderssen of The Globe and Mail wrote, is that most of the time our doctors do get their diagnoses right.
“But about one-fifth of the time, something is missed or conclusions are reached too quickly. Here’s how it can happen, and how a patient can help prevent it: Your doctor steps into the room, and already she has made a preliminary scan: your gender, your weight, your demeanor. She may have glanced at the chart with the nurse’s note and be considering two or three diagnoses, suggests Harvard medical professor Dr. Jerome Groopman, the author of ‘How Doctors Think’. It takes doctors, on average, 18 seconds before they interrupt a patient, which means facts in a patient’s history are often missed.
“Be as specific as you can about your symptoms. Write the details down if you need to keep them straight. Make sure you know your medications and the amounts you are taking, so the doctor doesn’t have to spend time figuring it out based on your ‘little white pill’ description.”
* Thanks to paramedic/fire captain Tom Bouthillet for telling me about the Circulation paper.
NOTE FROM CAROLYN: I wrote more about diagnosis and misdiagnosis in women’s heart disease in my book “A Woman’s Guide to Living with Heart Disease“ published by Johns Hopkins University Press in 2017. You can ask for it at your local library or favourite bookshop, or order it online (paperback, hardcover or e-book) at Amazon, or order it directly from my publisher (use their code HTWN to save 20% off the list price).
.
(1) Roxanne Pelletier et al. Sex-related differences in access to care among patients with premature acute coronary syndrome. Canadian Medical Association Journal. March 17, 2014 cmaj.131450 10.1503/cmaj.131450
( 2) Frederick A. Masoudi et al. Implications of the failure to identify high-risk electrocardiogram findings for the quality of care of patients with acute myocardial infarction: results of the emergency department quality in myocardial infarction (EDQMI) study. Circulation. 2006; 114: 1565-1571
(3) Pope JH, Aufderheide TP, Ruthazer R, et al. Missed diagnoses of acute cardiac ischemia in the emergency department. N Engl J Med. 2000; 342:1163-1170.
(4) E. James Potchen. Measuring Observer Performance in Chest Radiology: Some Experiences. Journal of the American College of Radiology. Volume 3, Issue 6 , 423-432, June 2006
See also:
“The ECG told the whole story, but nobody listened: ECG interpretation skills are critical to patient outcomes” via Dr. Stephen Smith’s ECG Blog
Cardiac gender bias: we need less TALK and more WALK
How can we get heart patients past the E.R. gatekeepers?
Misdiagnosis: the perils of “unwarranted certainty”
Heart attack misdiagnosis in women
Seven ways to misdiagnose a heart attack
Yentl Syndrome: cardiology’s gender gap is alive and well
When your doctor mislabels you as an “anxious female”
The sad reality of women’s heart disease hits home
Mayo Clinic: “What are the symptoms of a heart attack for women?”
Stress test vs flipping a coin: which is more accurate?
.
Q: Have you had an EKG that missed your ultimate cardiac diagnosis?
.

For about 2 years I’ve had chest pains that radiate between my shoulders and right shoulder sometimes it last 5 minutes, sometimes an hour. I’ve had EKGs done and a stress test and was told it could just be anxiety or acid reflux.
It can get pretty painful at times, I just don’t know what to do with myself. Heart disease runs on my mom’s side with the women especially, my mother had a heart attack about 4 years ago at 43 years old. I don’t know if I should get a second opinion, or do these test say enough that I would just be wasting my time doing so?
LikeLiked by 1 person
Hello Jessica – I’m sorry you’re having these distressing symptoms. I’m not a physician so can’t comment specifically on your experience, but I can tell you generally that getting a second opinion is always a reasonable option if your symptoms continue or get worse. You may also be a good candidate for starting a Symptom Journal. Just record the date, time of day, how long symptoms lasted, detailed description of the symptom (sharp, stabbing, dull, etc), what you were doing/feeling/eating in the hour or so leading up to the start of symptoms, what you tried doing to relieve symptoms, and what worked/didn’t work, etc.
Often a pattern can begin to emerge with your Journal to help you and your physician solve this diagnostic mystery. Right now, you just don’t know if these symptoms are heart-related or not. It’s quite common, for example, among people who have a family history of cardiac events at a young age like your Mom did, that every distressing symptom is interpreted as cardiac. But something is causing these symptoms – so if a doctor suspects acid reflux for example, were you given a diagnostic and treatment plan for that diagnosis?
Good luck to you – take care, and stay safe. . . ♥
LikeLike
Thank you!!
My doctor never actually did any test for acid reflux and anything after they just kinda told me that’s what it could be because my EKG and stress test were normal. I’ve also had issues with my blood pressure it’s either higher or low, my doctor asks me if I feel okay and I do so they said I’m fine if I don’t have any symptoms with the high or low blood pressure!!
I’ll be sure to start a chart and hopefully they can figure something out that helps with these pains I’ve been having – again thank you!
LikeLiked by 1 person
Here’s more info about that Symptom Journal for you – best of luck, Jessica. . .
LikeLike
One day, out of the blue, I get a call that my Mama was in the hospital. She had fainted 3x and broke both feet. She was at the hospital and her identical twin sister asked the dr to pls check her heart, even though both EKG and stress tests all came back normal. They couldn’t justify doing the heart cath until our family history was given. They decided to do it and found she was blocked, widow maker, and would have died if she had been sent home.
After double bypass, surgery on one of her feet, a month stay in the hospital later, she is better.
My worry is, HOW can doctors miss something as serious as this? I know all the excuses that have been told to me, but bottom line is, how as a woman, can you trust ‘tests’ whenever they are wrong and doctors dont listen to the patients saying how weird or off they feel.
Maybe if they started listening more, there wouldn’t be as many deaths. Not everyone falls into the perfect percentile that doctors seem to live by. Our whole family could have lost her if it wasn’t for this one doctor listening to the family history, going off our ‘gut’ that something was off.
They were treating her broken foot only, never once getting to the underlying question of WHY she was fainting in the first place, until my Aunt said something. That’s just scary to me as that’s what they should have focused on in the beginning. Why did she faint? Her broke foot was from the fall, yes, but why did she fall? That’s what these doctors need to start looking at, the true, underlying reason why this patient is there to begin with and getting a diagnosis for THAT!!
I’m beyond grateful that she was saved, couldn’t even imagine anything else, but we would have, we really would have with no family intervention. God and family saved her life first, then God helped the doctors’ hands do what needed to be done to save her for longer.
LikeLiked by 1 person
Hello Kristina – first, how fortunate that your mother was finally appropriately diagnosed and treated!
There has been a lot of research on cardiac misdiagnosis, particularly among women. It is so discouraging.
I just read a frightening case study this week of a woman in her 50s who was misdiagnosed in Emergency despite alarming symptoms. This report, published in the journal Patient Safety Network, summarizes several key recommendations for preventing multiple misdiagnoses. This kind of examination, after the fact, is rare.
One of the problems is that there is NO requirement for mandatory reporting of diagnostic error. NONE! Which means that none of the lessons learned in your own mother’s case will be shared, reviewed at Grand Rounds, taught to med students or otherwise used as a teachable opportunity to help prevent another patient suffer this dangerous close call.
We also know that women are significantly more likely to be misdiagnosed in the middle of a cardiac event compared to our male counterparts.
In your mother’s case, she had at least two things that worked against her chances of an appropriate cardiac diagnosis:
1. “normal” cardiac tests (not uncommon in women because virtually all cardiac diagnostic testing for decades has been researched on (white middle-aged) men
2. an acute and obvious non-cardiac issue (her feet)
Sounds like her puzzling fainting episodes weren’t even on their radar at first. Understandably, doctors are trained to address the most clearly obvious crisis in front of them, even though it is possible to have more than one medical crisis going on – as your family has learned firsthand.
Your story is also a good example of WHY women (and their families) MUST speak out when troubling symptoms are not being taken seriously.
Hope your mother is doing better each day, and recovering uneventfully.
Take care, stay safe… ♥
LikeLike
My name is Margaret Whyte, I am 72. Yesterday I went to my Doctor as I was having pain on the left side of my breast also feeling nauseated, sweating, pins and needles and numbness.I had an ECG done and it was ok, which did surprise me. Today the pain is still there and I just don’t feel 100%. What if I still have this pain in 4 weeks? What do you advise? Really tired. Thank you.
LikeLiked by 1 person
Hello Margaret – I’m not a physician so cannot advise you on your specific situation, but I can tell you generally that anybody experiencing distressing symptoms that are not “normal” (meaning that you have never experienced this particular combination of symptoms before, and especially if symptoms worsen over time), it’s always a smart idea to seek a medical opinion. You don’t need to wait 4 weeks.
Right now you just don’t know if your symptoms are heart-related or not, but SOMETHING is causing them. Good luck to you in solving this mystery!
LikeLike
On December 27, 2018 I called 911 to transport me to the hospital because I was positive I was having a heart attack.
The paramedics did an ekg and only saw a small abnormal result. At the hospital they did 2 ekg’s and the doctor did not feel it was a heart attack. She gave me a numbing liquid medicine to drink to see if the pain would subside which it did not. The nurse kept saying it’s a heart attack but the doctor was not convinced. Finally the second blood test came back with extremely high enzyme levels. My left rear artery was 100% blocked and the cardiologist was surprised I survived the attack. My blood pressure is always low, my cholesterol is always good and I am 5’ tall and 100 pounds so my BMI is great!
No explanation as to why someone who is great in all categories, eats proper and exercises would have a heart attack. I had crushing pain in the right side of my chest, jaw pain, nausea and sweating.
LikeLiked by 1 person
Hi Melinda – what a shocker this must have been for you (and for the ER staff who missed your diagnosis).
Your case illustrates the importance of doing serial cardiac enzyme blood tests (usually 2-4 hours apart) because it can happen that the first test result looks “normal” but the second one taken a couple of hours later shows significant enzyme levels.
You are in very early days still so it will take some time to heal psychologically and physically. Take care and keep learning all you can about your new diagnosis….
LikeLike
Is being 24 too young to have symptoms of a heart attack?
My chest and my upper back have been hurting down to my left arm.
LikeLike
Hello Cynthia – I’m not a physician so can’t comment on your specific symptoms. It’s possible – but certainly not common – to see women your age with heart disease. Talk to your doctor about your symptoms.
LikeLike
I am a 34year old female that like you was told that it was GERD and sent home multiple days in a row. It wasn’t until my enzymes rose after having a heart attack while laying in the ER, being completely ignored except for being told to stop hyperventilating (from pain) because I would make it worse, did they finally have a cardiologist come see me. This was my third ER visit, 5 EKGs, a stress test and 2 chest x-rays. The cardiologist took one look at my neck and sent me straight to the cath lab. They found my main artery clogged 99% and my heart was only pumping at 27%.
I now have a stent as well. I am diabetic, but have cholesterol levels of 140, actually fairly low. Your article hit home on so many levels. I feel less alone. I have all of the classic systems due to the locked hurting left arm to the distended vein in my neck and still no one in the ER listened or even believed.
I beg any woman of any age: be proactive in your health care. Don’t believe they know it all. Fight for your health. My cardiologist told me that this was going to kill me. I am lucky to be here.
LikeLiked by 1 person
Very good advice, Nichole. So glad you were persistent and kept returning to that Emergency Department. Best of luck to you…
LikeLike
I went to see Andrew Wang, MD at Duke Medical Center Cardiology. I am having atypical chest pain & severe shortness of breath. He is willing to prescribe Isosorbide for the angina but the idea of a CT scan or MRI of the heart was politely dismissed.
I have a stent in the right ascending artery and another smaller artery with blockage. Before my stent, I infrequently had angina but now, it is a mild event several times a day. Sometimes the twinges hurt, sometimes they are mild. But they happen every day several times a day.
Yes, losing weight and doing cardiac rehab are good, helpful ideas. But I want to know what is causing the angina & for someone to try determining if there is another blockage.
Before I had the stent, the angina was not as frequent and not as noticeable. I feel I have been patted on the head and sent home with admonitions to lose weight, get in better shape & therefore, my heart/lung problems will get better.
LikeLiked by 1 person
Hello Mary – I’m not a physician so cannot comment specifically on your distressing symptoms, but I can tell you in general that there are a number of contributing factors to angina other than large blockages that require stenting. Has your doctor also considered a diagnosis of Prinzmetal’s (a spasm disorder) or coronary microvascular disease?
When I was at Mayo Clinic, I met another heart patient there who had been happily living with severe angina for many years. She was also a keen tennis player. She regularly used her nitro spray as a preventive measure. Nitro is a vasodilator that works much like Imdur (isosorbide) to help her get through the day, including a dose before starting each game, then stopping halfway through the game to sit down, take another spray, wait five minutes, and then resume playing. I was stunned by her story at the time because she treated this as just a ‘normal’ part of her daily life.
If your isosorbide pill (or any other drug) is failing to manage your daily symptoms, talk to your doctor about either changing the dosage or changing meds.
LikeLike
Thank you for your stories. I am a 55 year female, with no previous heart problems. For the past 2 months, I am experiencing very strange symptoms (irregular heartbeat, squeezing feeling, nausea, shortness of breath when I go 1 set of stairs and I am a thin non-smoker) and yet when I got to the ER yesterday, they dismissed me, because my ECG and the blood test are normal.
I am not a hypochondriac. I never went to the ER before. I have no history of running to see a doctor and I know something is wrong. What do I do now?
LikeLike
Hi Lana – I’m not a physician so cannot comment on your specific distressing symptoms. Right now, you just don’t know if these symptoms are heart-related or not – but something is causing them. You might find it useful to start logging your symptoms: write down what time of day, what you’re doing when they happen, what have you been eating beforehand, how long each episode lasts, etc. And do not hesitate to go back if your symptoms get worse. Meanwhile, please make an appointment to see your own physician so these written incidents can become part of your health record. Best of luck to you…
LikeLike
It was an interesting contrast between my husband’s physical exam and mine. I had a heart attack 12 years ago this summer; at my last visit to the doctor, I got one page (standard letter size) printed out for my EKG. It took longer to set up the machine, than to run the actual test.
MY husband, who has never had any heart symptoms at all in his entire life, got six pages. We were having annual physicals with the same doctor, same staff, same date, same EKG machine. Granted I go to the women’s cardiology clinic at the state university, but that’s still quite a difference between an aging woman’s physical, and an aging man’s.
My significant changes may not have even shown up in those couple of seconds. Oy vey!
LikeLike
Hi Suze – that’s a pretty compelling difference within exactly the same family and within the same facility – and particularly questionable given that one of you already has a history of cardiovascular disease (which is of course a known risk factor for future cardiac events). If anything, you’d expect they’d be especially diligent in doing more careful testing with YOU, the actual heart patient. “Oy vey!” is right!
LikeLike
Thank you, Carolyn, for all that you do.
To make a long story short, my husband was so upset that he called the cardiologist at the university clinic. She asked for the name and address of the PCP, and was going to send off a letter about the neglect of female patients. She also said that with all of the articles and research appearing in medical journals, there is no reason at all for ANY physician in practice today to be ignorant of women’s cardiac issues.
(She sometimes says that if she were in charge, every doctor on earth would have a week long seminar on heart disease in women with a difficult test at the end.)
LikeLike
Well, you just made my day. I love that reaction from your cardiologist, and I hope that letter was a smack upside the head for that PCP and all other docs who hear this story. Thanks for that part of the story!
LikeLike
I don’t think results of that study of radiologists can be told too many times. Especially the part about how the worst were the most confident and the best were the most uncertain.
Aside from confirmation bias, my own cardiac story points to yet another point of Dr. Groopman’s.
My EKG was abnormal on 3 of 4 indices. Along with my episodes of exhaustion and shortness of breath (extraordinary in anyone who works out as much as I do) it alarmed them enough to send me to the ER and give me an angiogram the next morning, which was 90% clear. So far, so good. Chalk one up for the HMO.
But at that point the cardiologist lost all interest in my symptoms (which still popped up out of nowhere). Some triathletes have similar EKGs, and he insisted that the EKG was just my Normal, like my very low heart rate, due to years as a runner, even though that was some time ago.
When I did more research and pointed out that Apical Hypertrophic Cardiomyopathy would explain the EKG as well as my symptoms, he smiled tolerantly. For several years the cardiologist and one PCP after another smiled tolerantly and told me how very rare that would be. When I reminded them that I have already survived a cancer that is far more rare, the smiles became rigid. They reassured me that “Dr. X” or “Dr. W” is an excellent doc and that was that. Among the list of indicators for AHCM is Sudden Death.
Then I changed PCP yet another time (see “Anxious Female”) and decided to revisit the heart issues.
My new doc asked a cardiologist she really respected to read my echocardiogram, and he determined that I do have Apical Hypertrophic Cardiomyopathy, consistent with previous echo and all previous EKGs. In fact, a pretty textbook case (my new cardiologist tells me) missed by all previous docs at the HMO.
Dr. Groopman tells us that docs are trained: “When you hear the sound of hooves, look for horses, not zebras.” And too many docs behave as though rare means impossible in that person before them.
But some of us really are zebras, even again and again.
LikeLike
Hello Kathleen,
It’s usually a bad sign when a cardiologist loses all interest in your symptoms on the basis of a “normal” diagnostic test. “Normal” does not mean one’s disease politely goes away.
Right now, a dear friend is in ICU on life support with brain swelling of sudden onset and unknown cause while neurologists, radiologists and other specialists report that they are “mystified” as test after “normal” test reveals little to solve the mystery. Yet they’re continuing to aggressively pursue a diagnosis. SOMETHING is causing this and they’re trying desperately to figure out what that is.
Yet in cardiology, a “normal” diagnostic test can make some physicians forgetful – as in, they seem to forget about the symptoms that were distressing enough to bring us to seek medical care in the first place.
And as if that weren’t bad enough, they “smile tolerantly”. Arrrrgh….
LikeLike
So sorry about your friend, Carolyn, and good to hear that the team looking after her (or him) has not thrown in the towel but is aggressively pursuing a diagnosis. So often real life conditions take a different form from “type”. We hope for the best.
LikeLike