 Most of our medical visits start with some variation of this opening question: “Why are you here today?” Connecting with and understanding patients thus requires doctors to listen to what’s called the patient narrative. The importance of really hearing this narrative is beautifully described by U.K. physician Dr. Jeff Clark, writing in the British Journal of General Practice. But the problem, as Dr. Clark reminds his peers, is that patients and doctors see the world in very different ways. He also warns that the stories patients tell their physicians about why they’re seeking medical care may all too often be seen by doctors as merely a time-wasting distraction from “getting to the bottom of things.”
Most of our medical visits start with some variation of this opening question: “Why are you here today?” Connecting with and understanding patients thus requires doctors to listen to what’s called the patient narrative. The importance of really hearing this narrative is beautifully described by U.K. physician Dr. Jeff Clark, writing in the British Journal of General Practice. But the problem, as Dr. Clark reminds his peers, is that patients and doctors see the world in very different ways. He also warns that the stories patients tell their physicians about why they’re seeking medical care may all too often be seen by doctors as merely a time-wasting distraction from “getting to the bottom of things.”
The urge to get to the bottom of things may also help to explain what’s known as “The 18-Second Rule”.
This stems from a well-known 1984 study by Beckman and Frankel published in the Annals of Internal Medicine in which researchers observed that patients were allowed to complete their opening statement about their problem in only 23% of physician interviews. The average time to interruption was just 18 seconds. And, sadly, this study’s findings on “not listening” have been replicated by several others.
Good listening skills, on the other hand, have sometimes been described as “humble inquiry”, as outlined in the book of the same name by social psychologist Dr. Edgar Schein. (1) It’s about asking questions from an attitude of genuine curiosity and interest about the other person, and specifically what’s called “curious listening.”
Dr. Jay Baruch is a Rhode Island Emergency physician and author of Fourteen Stories: Doctors, Patients, and Other Strangers. He advised physicians recently to start thinking about patient stories like creative writers would do:
“Healthcare providers should be story experts.
“Thinking more creatively makes us more accepting of challenging stories.
“In the narrative disaster zone of the emergency department, patients’ stories often feel like a first draft, and first drafts – for most of us – are typically raw and messy. Patients’ stories are complicated, intensely personal and disorganized.
“Our patients come to us sick, frightened, tough and maybe distrusting. They face a daunting task that we sometimes take for granted: to construct deeply personal narratives for nurses and physicians who, until that moment, were complete strangers”
“We must listen to the patient’s story if we wish to help them.”
Nurses are just as important as physicians in honouring the patient’s story, according to U.K. researchers who reported this on their study called “We Listen, But Do We Hear?” (2)
“Patients’ perspectives on their illness and care are increasingly recognized as the focus for the organization of health care, yet patient stories are rarely examined on their own.
“Mostly, they are dissected for data, and so the impact is lost. Nurses can play a critical role in optimizing the power of the story in the patient’s journey towards physical and psychological healing.”
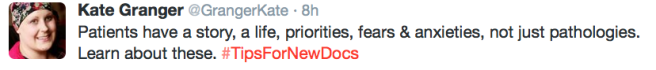
Dr. Kate Granger is a U.K. physician who also happens to be a patient living with terminal cancer.* Here’s her Twitter advice to new docs from both a doctor and a patient’s perspective:
Her countryman Dr. Clark also believes that listening thoughtfully to patient stories is a critically important part of a good patient-centred clinical consultation. And he also knows that, while the patient has a narrative, so does the doctor – and physicians could enlist this in their tool box to share health information with the patient.
“We are, after all, educators and – as BF Skinner says: ‘Education is what survives when what has been learned has been forgotten.’
“Saying to the patient: ‘You must stop smoking’ might work, but how about using a little tale and fixing it into their narrative, such as: ‘You were telling me earlier what happened to your dad because of smoking? It would be a shame to give your kids the same memories.’
“Doctors need to weave knowledge into the narrative if the patient’s understanding is to be appreciated and changed.”
Finally, it’s important to say here that my story as a patient is just one of many stories about me. It’s why people living with diabetes often cringe at being called “diabetics”, those living with asthma similarly cringe at “asthmatics”, those living with epilepsy . . . well, you get my drift.
When I was hospitalized with a heart attack, I overheard Emergency Department staff referring to me as “the MI in Bed 8”. To use a medical diagnosis as a shortcut label to describe another human being is to strip away that which makes the human unique, and to increase the risk that you think you know that human by the time those 18 seconds of listening are up.
♥
(1) Schein, E. (2013). Humble inquiry: The gentle art of asking instead of telling. San Francisco: Berrett-Koehler Publishers, Inc.
(2) Hawkins J. “We listen but do we hear? The importance of patient stories.” British Journal of Community Nursing. 2006 Sep; 11(9):S6-14.
♥
*UPDATE: Dr. Kate Granger died on July 23, 2016 at the age of 34. Her terminal cancer diagnosis led her to launch the now-famous “Hello My Name Is” campaign to remind all health care providers to introduce themselves to patients. Her obituary is here.
.
See also:
- The ’18 Second Rule’: why your doctor missed your heart disease diagnosis
- Just not listening – or “narrative incompetence”?
- Is your doctor paying attention?
- Emotional intelligence in health care relationships
- Tell me a (heart attack) story
- Empathy 101: how to sound like you give a damn
.
Q: Can already-rushed doctors take the time to engage in listening to the patient narrative ?
.

Reblogged this: HEART SISTERS
LikeLike
There is much to think about in this post. I’m glad Marie pointed us over.
~Catherine
LikeLike
Thanks Catherine, and thanks Marie for pointing me out to the readers of Journeying Beyond Breast Cancer!
LikeLike
Reblogged this on Journeying Beyond Breast Cancer and commented:
“Thoughts on patient narrative wonderfully expressed as always by Carolyn Thomas.”
LikeLike
Love, love, love this! And your timing is perfect. I am putting together my slides for my Medicine X talk next month on…the importance of patient narratives.
It is a challenge for me as I only get 5 minutes to speak and as you know there is just SO much to say on this topic. To enter into an experience which often lives outside the clinician’s own understanding depends upon finding an entry point. Stories can be that point of entry. Stories offer opportunities to put patients at the center of their care, allowing them to become coauthors of their health narrative – to quote Jay Baruch again, “story becomes the ground that patients and healthcare professionals travel together”.
LikeLiked by 1 person
Thanks Marie – and especially for reposting this essay on your site. You are so right – five minutes is impossibly tight for such an important topic! You could go on for days, really… Best of luck at Stanford – I’ll be watching you online this year. 🙂
LikeLike
Totally agree with you. I am fascinated by this topic and also how patient engagement is being affected by doctor’s use of technology (see here: http://huff.to/1sFEOgj). It seems that there are so many barriers to communication and hearing the “patient narrative” in full these days!
LikeLiked by 1 person
Great article, Dana – thanks for sharing it here.
LikeLike