
by Carolyn Thomas ♥ @HeartSisters
Part 1 of a 3-part series about pain
I was thinking about the freakish nature of pain the other day. I think about pain quite a bit, actually, given the frequency with which I now experience the ongoing symptoms of coronary microvascular disease. But when the first alarming warning signs of a heart attack struck out of the blue while I was out for a brisk pre-breakfast walk, the reality was not at all what I would have ever imagined a heart attack to feel like. And because I was clueless, I believed the Emergency Department physician who’d misdiagnosed me with acid reflux and sent me home that same morning.
Besides, I’d always assumed that any person having a heart attack would clutch at his chest in agony (in my mind, this person was always a white middle-aged man – because that’s the image we see in the media) before crashing down onto the floor, unconscious. (I did not know then that this scenario is NOT a heart attack, by the way; it’s called sudden cardiac arrest, and yes, in well over two-thirds of cases, it does happen to men).
But on that day, I was fully conscious and able to walk and talk and think throughout my visit to Emergency. Thus my mistaken assumption was also that the Emergency doc was correct – despite my textbook symptoms like central chest pain, nausea, sweating and pain radiating down my left arm.
My cardiac symptoms later returned (of course they did!) and increased over time until finally, unable to stand them any longer, I returned to the same Emergency Department. This time, I was greeted by a different doctor plus a new and correct diagnosis of myocardial infarction (heart attack) caused by a blocked left anterior descending coronary artery – the so-called widowmaker heart attack.
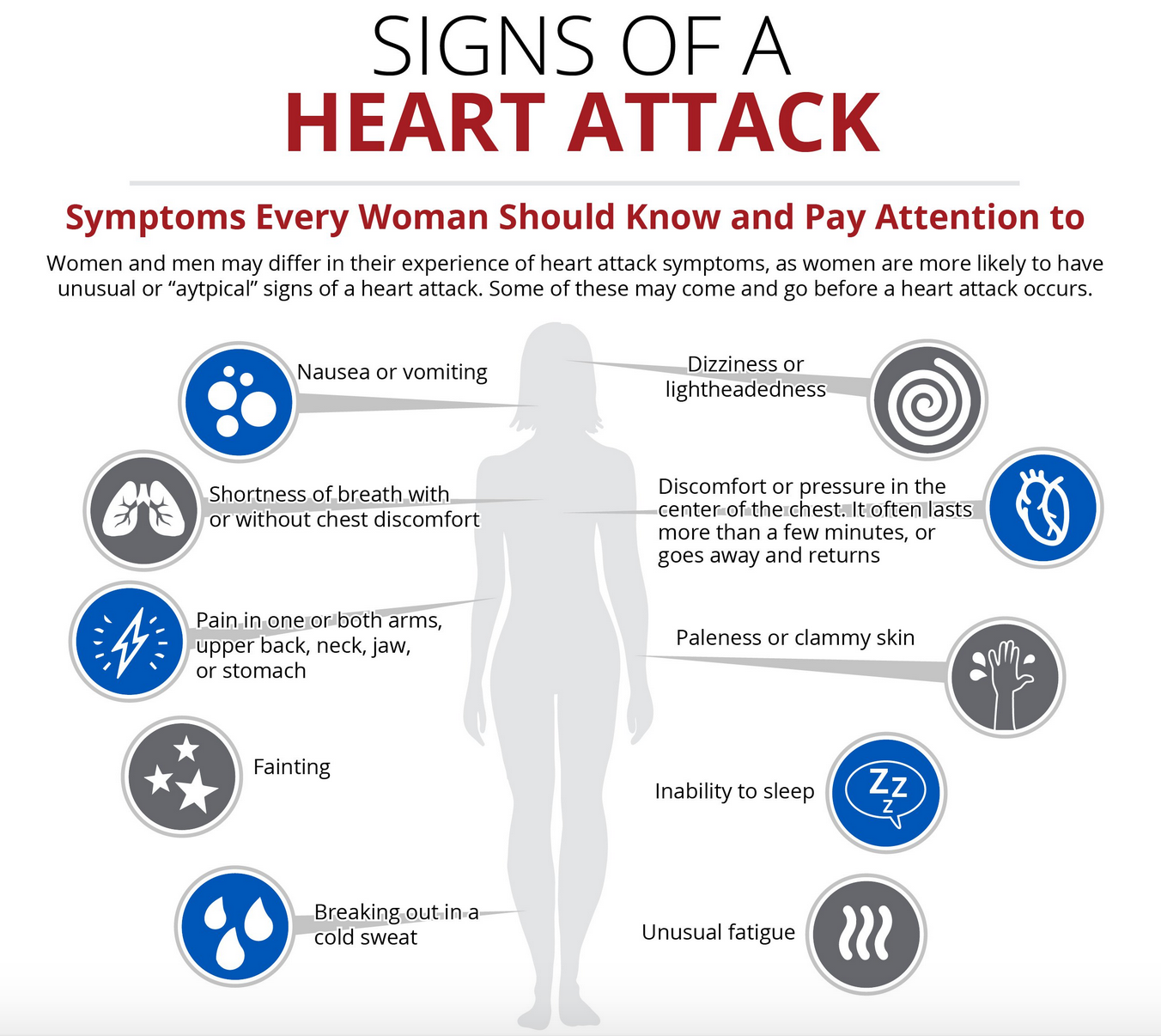
And if you’re having a heart attack, distressing warning symptoms can actually be felt anywhere between nose and navel. When your heart muscle cells begin to run out of oxygen because of a blocked artery or a spasm preventing oxygenated blood from feeding that muscle, they begin to send off signals of pain throughout the nervous system. But your brain may also confuse those nerve signals with signals coming from the arm (or the jaw, shoulder, elbow, neck or upper back) because of the nerve proximity. That’s what referred pain is. It happens when pain is located away from or adjacent to the specific organ involved – such as in a person’s jaw or arm, but not necessarily in the chest.
As I wrote here, a heart attack may cause a sensation of pain to travel from your heart to your spinal cord, where many nerves merge onto the same nerve pathway. So your arm may be perfectly fine, but your brain thinks that part of the pain is in the arm (or the jaw or the shoulder or the elbow or the neck or the upper back) calling out for help.
This is more common when heart attack occurs in older people or those who live with diabetes. But even using the words “chest pain” to describe this heart attack symptom might be tricky. Many women may not even use the word “pain” to describe their cardiac chest symptoms, but instead use words like pressure, ache, heavy, suffocating, full, tight or burning. See also: Downplaying symptoms: just pretend it’s NOT a heart attack
And remember that at least 10% of women having a heart attack experience no chest symptoms at all.(1) None. Nothing. Zip. Zero. Nada.
What I’ve learned during my own cardiac adventure was this:
There’s pain, and then there’s pain.
Pain in general is actually nature’s way to protect our bodies. Pain has a way of attracting our focused attention in a laser-like fashion, warning us that something might be very wrong. For heart patients, there’s the initial scary pain of a cardiac event, and there can also be ongoing pain following that event. If you’ve had one or more coronary stents implanted, for example, you may experience what we call “stretch pain“ for a while. Although it’s common for heart patients to experience some residual pain following a cardiac intervention, such symptoms may also indicate a serious complication – so call your doctor if pain persists or gets worse instead of better over time.
Since my heart attack, I’ve had lots of time to consider the amazing mind-body relationship of pain. Because of ongoing and debilitating cardiac symptoms (and accompanying daily pain symptoms that feel virtually identical in intensity to my initial heart attack pain), I now see a pain specialist regularly at our Regional Pain Clinic (visits I’ve written about here, and will write about again when I cover the subject of pain self-management in the second part of this 3-part series on cardiac pain).
If you’re living with the ongoing pain of angina, by the way, please ask your physician for a referral to your local Pain Clinic if your community has such a resource.
The physicians, nurses, physiotherapists, occupational therapists and psychologists who work there are true experts in the nature of what pain is and how our bodies interpret that pain. These folks know their stuff. Most other pain patients I see there are living with some type of chronic pain caused for example by arthritis, migraines, injuries, surgical complications, etc.
And where I live, all of my visits/treatments in the Pain Clinic (as well as all cardiology follow-up tests, hospital stays, and doctors’ appointments) are free. Thank you Canada, a.k.a. commie-pinko land of socialized medicine according to our American neighbours.
My particular kind of ongoing chest pain is generally tolerable most days as long as I pay careful attention to:
- medications (remember, heart sisters, that “Nitro is your friend!“)
- regular daily exercise (as Kentucky cardiologist Dr. John Mandrola likes to say: “You only have to exercise on the days you plan to eat!”
- the portable TENS unit I wear clipped to my belt from dawn to dusk
- naps
- keeping a strictly cautious eye on my daily stress levels
- ongoing care from our Regional Pain Clinic staff, an expert pain specialist, and most importantly the free pain self-management programs offered there.
Meanwhile, here’s my best advice if you or somebody you care about experiences what feels like heart attack symptoms:
- Call 911. Do not let anybody drive you to Emergency. Do not drive yourself.
- While you’re waiting for the ambulance to arrive, chew one regular full-strength (300-500 mg) uncoated aspirin (or generic ASA) washed down with water – provided that you are not allergic or already taking bloodthinning meds.
♥
(1) S. Dey et al, “GRACE: Acute coronary syndromes: Sex-related differences in the presentation, treatment and outcomes among patients with acute coronary syndromes: the Global Registry of Acute Coronary Events”, Heart 2009;95:1 20–26.
..
Q: Have you ever had an example of freakish pain?
NOTE FROM CAROLYN: I wrote much more about identifying cardiac symptoms in Chapter 1 of my book, “A Woman’s Guide to Living with Heart Disease”. You can ask for it at your nearest library or local bookshop or order it online (paperback, hardcover or e-book) at Amazon, or order it directly from my publisher, Johns Hopkins University Press (use the code HTWN to save 30% off the list price).
See also:
Part 2 of this 3-part series: Brain Freeze, Heart Disease and Pain Self-Management
Part 3 of this 3-part series: Chest pain While Running Uphill
What is causing my chest pain?
The chest pain of angina comes in four flavours
How does it really feel to have a heart attack? Women survivors tell their stories
Why does your arm hurt during a heart attack?
How women can tell if they’re headed for a heart attack

My oddball symptoms that led to a diagnosis “by exclusion” of coronary microvascular disease keep me guessing. My first episodes last year included chest pain radiating to my jaw. I was “too busy” to get it checked out, although I had heard that jaw pain can be from the heart. Last night I felt just the jaw pain –both in the upper and lower jaw–but no chest pain. The jaw pain was localized to only the front of my jaw, above my front teeth and in my front lower jaw–not at all on the sides. Weird. It lasted about 45 minutes. It has gone away, so I doubt that it was dental in origin. I don’t have a cold or other illness. I had gone for a walk an hour before the jaw pain, and I was simply seated at my computer at work when this came on. I never get symptoms from exertion.
My question: can one have only jaw pain without concurrent chest pain that is actually related to the heart? I told myself that if the chest pain and jaw pain coincided, then maybe I would get it checked out at a hospital. I decided not to go to the hospital last night. I could just imagine what an ER doctor would think: what a hypochondriac, coming here with just pain in her jaw! I know you wisely refrain from giving medical advice, but I wondered if your readers with heart disease have ever had just jaw pain with no chest pain.
My angiogram last December showed only 50-60% narrowing of my LAD. The interventional radiologist concluded that I have endothelial dysfunction/coronary microvascular disease. He said I have unstable angina. He said he does not need to see me again. My primary care doctor thinks it wise to go out of state to get further testing. I can’t take typical heart medications since I have very low blood pressure (often in the 80ish over 40-something range). So no nitro or beta blockers for me. I have experienced infrequent night-time shortness of breath while sleeping (but no sleep apnea diagnosis after a sleep lab test was negative at the hospital). The night before this jaw pain episode yesterday, I did have some shortness of breath while sleeping, but it was not alarming.
At times this is a frustrating situation. However, I choose to be grateful, not resentful. Clearly, many people have way worse symptoms than I have had thus far. I can function just fine. I don’t want to be a whiner nor waste medical resources. But my family reminds me to not discount what might be warning signs. It is just so confusing to sort out what might be angina and what might be a message from my heart to get to the hospital.
Thanks for creating this amazing resource! You are a truly generous, compassionate person who is making a difference in our lives.
LikeLiked by 1 person
Thanks so much for your kind words, Marie. You’re right, I’m not a physician so cannot comment specifically on your diagnosis (although I am wondering what remedy the doc who diagnosed you with stable angina is recommending, given that you can’t take nitro, etc?)
But I can also tell you generally something I just learned yesterday while writing an upcoming blog post on jaw/teeth symptoms linked to heart disease (perfect timing for you). And YES a number of researchers have suggested that jaw/tooth pain without and without chest pain has been identified in heart patients – it’s not common, but has been identified (what health care professionals call “orofacial pain of cardiac origin” – I was surprised how many studies have focused on this specific subgroup of symptoms). For example: “There are published clinical cases of patients who have undergone unnecessary dental extractions or have been prescribed pain medications due to misdiagnosis, without curing the orofacial pain.”
LikeLike
The interventional cardiologist wrote in my hospital report after my angiogram that I have unstable angina (not stable). He had no advice for me in terms of medications. He said antioxidants are beneficial for endothelial dysfunction, but he did not suggest supplements–just eating a Mediterranean diet. I eagerly await your next blog posting on orofacial pain of cardiac origin. I appreciate knowing that one can have jaw pain without accompanying chest pain that might be provoked by cardiac issues. This can be such a mystifying disease!
Thank goodness we have someone like you with such stellar research skills to sleuth out the clues and point us to solid information. I am so sorry you had to come by your passion for heart health education via calamitous events like your own heart attacks. You are rock-steady, rational, and laser-focused on seeking the truth and summoning us all to become our own best advocates for our personal health.
I have been a determined supporter of my own family’s needs, and now it is not so easy to switch gears. I was the “roommate” who slept in hospital rooms during my loved ones’ illnesses or surgeries. I gladly went with them to their medical appointments, researched illnesses, etc. as I advocated for my parents and brothers during their difficult journeys. I lost five close family members in three years’ time: three brothers and both of my parents. My oldest brother and my father died two days apart in different hospitals. It was quite a workout, since we did not want to leave either one to die alone. I was just so grateful to be able to be present to help even in a small way. I am used to being the one who helps, not the “helpee.”
My sons remind me that I need to quit “being a Norwegian,” which is code for being stoic like my husband’s family has been when health problems surfaced. I am far from Norwegian, although I have learned how to make krumkake and fish cakes (and even valiantly ate lutefisk as a respectful daughter-in-law of a Norwegian immigrant). My Native American background reminds me that I should live each day with an open spirit. When the time comes, I want to face death with an attitude in tune with the saying, “Today is a good day to die.”
But for now, it is a good day to live, and so I will do so with a grateful heart.
LikeLiked by 1 person
You raise so many good points, Marie (e.g. switching from being the helper to being the “helpee”). Love that “quit being a Norwegian” advice from your sons!
And you’re absolutely right – today IS a good day to live…
LikeLike
I get ventricular tachycardia and pain in my right shoulder with that sometimes. Our bodies can be so mysterious.
LikeLiked by 1 person
Yes – it is strange, but true!
LikeLike
Yes, women can have all types of ‘heart pains’. I am a survivor of an Atrial Myxoma. In my 19th year of surviving the removal of that tumor in my heart. As a young woman, it never occurred to me that something could be wrong with my heart.
Chronic fatigue, severe pains in my chest when climbing steps, and all the while no doctor could find what was wrong. I simply was diligent because I knew something was not right 🙂
Then I had the blessing – finally – of a doctor who believed me. First I had a stress test on a treadmill, every time the pain came, my doctor asked me where it was. Then he gave me a sonogram. When he looked at it – he knew something was blocking the blood trying to go into my heart!
Yes, we must be know our bodies, network, make sure to learn more about heart disease. Thank you for this wonderful blog. I hope my story helps someone!
I am a St. Francis, Brave Heart
LikeLiked by 1 person
Your story is a very helpful reminder that we must all be “diligent” when we have that same feeling – that “something is not right!” – until our symptoms are taken seriously. Best of luck to you…
LikeLike
Thank you! What a great source of information! I am so pleased to find it, and will follow-up on my blog about this very important health issue 🙂
LikeLiked by 1 person
Thank you for providing insight into what are generally very common misconceptions regarding heart disease. It’s important to raise awareness of any and all forms of symptoms when dealing with a range of disease that effects somewhere close to 30% of people alive today.
LikeLiked by 1 person
Agreed!
LikeLike
Carolyn,
Love the commie pinko socialized medicine bit! Bring it on!
For open heart surgery patients there is the pain of essentially, a broken sternum as well as the pain from all the attendant nerve and muscle damage. When you have heart problems of course all pain in the chest area makes you anxious. It took me a while to differentiate the surgical pain from heart spasms. And I still have random nerve pain 3 years later which always makes me reach for the panic button before I remember to take a deep breath and focus on the source.
LikeLiked by 1 person
Such an important point, Lauren: reaching for the panic button is the natural reaction to all chest pain. It does take time to learn how to be discerning and actually believe that not every twinge necessarily means a 911 speed dial. I still have the same amount of ongoing cardiac pain as I did years ago, but I’m getting so much better at taking a moment to observe and qualify it before I start to panic.
LikeLike
I have been so blessed because I have not experienced severe heart pain through 12 stents and one NSTEMI heart attack. My first symptoms in 2005 were breathlessness with any exertion. This continued to be my experience 4 times through 2005 and 2006, producing 8 stents.
Then, a seven year break where I simply took my medicine and gave it no thought. Things changed when I began having mild mid chest pain with exertion in 2013. I was scheduled to have a cath on a Tuesday, but didn’t make it, needing to call 911 and had the cath a day early. When you can’t get to the bathroom from your chair without mid-back and mid-chest pain, it’s time to call 911 even though Nitro is my friend. This time there were changes in my EKG. Two more stents.
Then in July 2014 stronger back and chest pain with some lab indication of the beginning of muscle damage. Two more stents.
I am well aware that at some point I will hear, “We’ve run out of ways to treat your symptoms/heart attack/whatever. And you need heart surgery.”
This does not prevent me from being thankful for my trip thus far.
LikeLiked by 1 person
Thanks Pauline for sharing your personal story here. And good advice about staying thankful for your care so far – what I’ve learned is that there is absolutely no advantage in worrying about the “what ifs” in life.
LikeLike