 by Carolyn Thomas ♥ @HeartSisters
by Carolyn Thomas ♥ @HeartSisters
Once discharged from hospital following my heart attack, I was gobsmacked by how physically frail I felt. Simply taking a shower meant a 20-minute lie down to recover. Just walking to the corner with my son, Ben, required me to clutch his arm for support. But it wasn’t only this new weakness that alarmed me. As a former distance runner, I felt suddenly afraid of any exertion that might bring on the horrific heart attack symptoms I’d so recently endured. That’s where cardiac rehabilitation (a 2-4 month supervised exercise and education program for heart patients) literally saved me. Cardiac rehab does indeed save lives. According to The American College of Cardiology (ACC):
“Women with coronary artery disease who completed a 12-week cardiac rehabilitation program were two-thirds less likely to die compared to those who were NOT referred to the program.
“In addition, the mortality benefits of this evidence-based program derived for patients with angina, or for those recovering from heart attack, coronary artery bypass graft or implanted stents appear to be much more striking in women than in men with the same condition.”
Yet despite the known evidence-based benefits of cardiac rehab for heart patients, participation rates are absolutely dismal – for many reasons. The most alarming reason is this one: a 2012 American Heart Association report suggested that doctors themselves are “a significant obstacle to cardiac rehabilitation participation”: only 20% of all eligible heart patients are referred by their physicians to cardiac rehab (1). We know this referral is critically important. As the ACC report explains, physician endorsement is one of the strongest predictors of full participation in cardiac rehabilitation. It’s also why Oregon cardiologist Dr. James Beckerman, in his book Heart To Start, is blunt in his assessment of those doctors who fail to refer their patients to cardiac rehab:
“It is bad medicine to withhold life-saving treatments, and many physicians are selling their patients short.”
Some researchers suggest that our physicians may simply be “unaware” that in current practice guidelines of all cardiovascular societies worldwide, cardiac rehabilitation for heart patients is a Class I recommendation (which means that a procedure/treatment should be performed/administered).
By comparison, as I’ve observed here, I’ve never heard of a cardiologist anywhere, at any time, ever who is “unaware“ of the routine prescription of DRUGS to every survivor of every possible cardiac event.
Yet even when informed doctors do prescribe a cardiac rehab program for their heart patients, we know that there are other obstacles, particularly for women, to both attendance and completion. See: Why aren’t women heart attack survivors showing up for cardiac rehab?
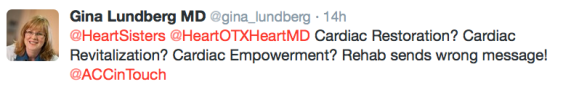
Cardiologist Dr. Gina Lundberg also wonders if perhaps even the name itself could be the culprit. Are the words cardiac “rehab” simply off-putting for some patients and their physicians?
For example, Dr. Gina (a Preventive Cardiologist & Clinical Director of the Emory Women’s Heart Center in Atlanta) tweeted this recently to me (@HeartSisters) and to Texas cardiologist and keen cardiac rehab proponent Dr. John Erwin III (@HeartOTXHeartMD):
.
 .
.
Should we change the name? As I like to do when faced with such a good question, I go straight to Real Live Patients, the women with actual firsthand experience of cardiac rehab. Here’s how some of my heart sisters feel about changing the cardiac rehab name:
♥
♥ “The name ‘cardiac rehab’ is called that because it’s cardiac rehabilitation. I don’t understand the name cardiac ‘rehab’ being offensive, construed as addiction rehab or anything other than calling it the appropriate name: cardiac rehab.” (heart attack, SCAD*)
♥ “My feeling – it is what it is. You can change the name to whatever you wish. It still is the same program. To me it didn’t matter the name, it was the benefits that I derived from it. Also, let’s face it, most of us knew the benefits of exercise prior to our heart issues. What we lacked was the discipline and/or the support of others in our quest to exercise.” (heart attack, double bypass surgery)
♥ ” The name ‘cardiac rehab’ helps me remember why I go, and it drives me on.” (heart attack, three stents)
♥ “I think the name is just fine. I only attended for about six sessions. It was good, but I had to pay $60 for each session and find a babysitter each time I went, so I had to stop.” (SCAD*)
♥ “My current cardiologist is not a heart failure specialist but continues to support my participation. He said that the name ‘cardiac rehab’ is a misnomer. The heart is not rehabbed by the exercise, but it improves the overall functioning of the body.” (heart attack, heart failure)
♥ “Cardiac rehab name is fine, it’s the cost and scheduled time of classes that are the problem. Cardiac rehab is scheduled during the day and so isn’t an option for those who have to work.” (mother of a SCAD patient*)
♥ “Maybe they should call it cardiac resurrection instead of cardiac rehab. Thankful to God every single day for my second chance. I pay for it out of my own pocket. I’m worth it!!!!!” (heart attack, SCAD*, cardiac arrest, four stents)
♥ “Hey, I like that term cardiac resurrection, that is kind of what it is. Maybe use a spa term like cardiac rejuvenation or cardiac retraining. Then we could call them personal trainers; we could look at it as training rather than rehabbing. Or maybe use the term cardiac education, because that is what it was, too: education in a subject that I knew nothing about. And it trained me how to live for the rest of my life.” (three heart attacks)
♥ “I personally think the term ‘rehab’ is a very big deterrent. It immediately conjures up images of drug addiction or of being completely incapacitated. I know that when I was referred to ‘cardiac rehab’, I had to deliberately make myself swallow my pride. Had it been termed something like cardiac recovery enhancement program, I might have had a much better attitude. Following my heart attack, I did go to our local cardiac rehab program and learned heaps. My cardiologist at that time offered me NO advice what so ever!!!!!” (heart attack, coronary artery spasm, coronary microvascular disease)
♥ “I have no problem with the label ‘cardiac rehab’, because that’s exactly what it was for me.” (heart attack)
♥ “There is no room for shame in the word ‘rehab’ whether it’s cardiac, addiction, pulmonary, etc. – they are all diseases. People in any kind of rehab are working at getting well. We are all so lucky that we get to go to any rehab that strengthens our minds, bodies, and souls. Focus on the getting well part.” (heart attack)
♥ “Funny story: I ran into someone on my way to my cardiac rehab class. They asked where I was headed. I said to rehab. Few days later a totally different person comments to my husband that they are not surprised I had a heart attack – with my drug use! I have personally recommended cardiac rehab to many people and always found myself having to explain it, so perhaps it is a question of changing the image it promotes?” (three heart attacks)
♥ “I don’t know why ‘rehab’ has such a negative connotation. If something isn’t right, it is rehabbed. And rehab is not just for addiction. There are many rehab hospitals that deal with physical illnesses. My daughter-in-law is a Physical Medicine and Rehabilitation physician. She works with head, spinal, and other injuries to help them recover. She does not work with alcohol or drug addiction as a primary concern. Rehab is a fast-growing area of medicine. I think the problem with the negative connotation may be in society’s problem with addiction and many persons’ inability to see addiction as an illness, not a choice.” (heart attack, sudden cardiac arrest)
♥ “I went to cardiac rehab for 36 visits. I don’t particularly object to the name.” (heart attack, quadruple bypass surgery)
♥ “There are a lot of older guys in my cardiac rehab. They’ve kind of adopted me as their cheerleader. They call the rehab ‘cheap life insurance’. I like the name ‘cardiac rejuvenation’. I can feel my arteries clearing up already!” (heart attack, stents)
♥ “The ‘rehab” name didn’t bother me – instead my favorite song to treadmill to became Amy Winehouse’s Rehab (No, No, No)!” (coronary artery disease, two stents, congestive heart failure)
* SCAD means Spontaneous Coronary Artery Dissection
.Thanks to my heart sisters who took the time to share their opinions and stories!
♥
.Q: Do we need to come up with a new name to replace “rehab”?
(1) Arena, R et al. Increasing referral and participation rates to outpatient cardiac rehabilitation: the valuable role of healthcare professionals in the inpatient and home health settings. A Science Advisory From the American Heart Association. Circulation. January 30, 2012
♥
NOTE FROM CAROLYN: I wrote more about the importance of cardiac rehabilitation – no matter what you call it! – in my new book, “A Woman’s Guide to Living with Heart Disease” (Johns Hopkins University Press, November 2017).
See also:
- Returning to Exercise (and Training) After Heart Surgery (THE best and most comprehensive overview on this topic I’ve seen yet, written by cardiologist and triathlete Dr. Larry Creswell; especially useful for heart patients who have been regular exercisers before their cardiac event and are wondering how to safely resume their routine)
- The surprising reasons heart patients don’t go to cardiac rehab
- Failure to refer: why are doctors ignoring cardiac rehab?
- ‘Women-only’ cardiac rehabilitation curbs depression for heart attack survivors
- Why aren’t women heart attack survivors showing up for cardiac rehab?
- Study: “91% discharged from hospital without care plan”
- Why your heart needs work – not rest! – after a heart attack
- Cardiac Rehab: Boosting Your Heart Recovery (article in US News mentions this blog)
.

Carolyn, I’m so behind in my blog reading, but I’m sitting here, finally trying to write the first of what I hope will be several posts about gentle exercise, and had to write this comment.
As a homecare physical therapist, I often visit folks who’ve just experienced some kind of cardiac event — bypass surgery, a heart attack, a bout of congestive heart failure, stent placement, pacemaker placement, atrial fibrillation, etc. etc. We are lucky here where I live to have both a wonderful outpatient cardiac rehab program and a pulmonary rehab program, both covered by insurance, at our local hospital. There is even door-to-door transportation provided. But I continue to be astonished that, in the first place, so many patients are not referred for homecare after such hospitalization, and, in the second place, that I often end up being the first person to inform them that outpatient cardiac & pulmonary rehab programs exist.
I don’t know why this is, really, but I do know that homecare PT is very helpful in getting people to start feeling normal again. We are trained to monitor vital signs before, during, and after exercise, often including a home telemed monitor that can transmit daily vitals to our specialist nurse back at our office.
Most of the time, I have to start very slowly and gently with patients. But even when they can only tolerate a minute of walking at a time, if they persist, they can almost always improve to that magic six-minute walk that is generally the baseline requirement for being accepted into an outpatient program. I think that patients themselves are often the best advocates for asking for these services. If they ask for homecare services when they are discharged from the hospital, they are often much more likely to be referred to an outpatient program (because we ask their doctors to do so!), to be physically ready for them, and to be receptive to them.
Now, back to that blog post…
🙂
Kathi
LikeLiked by 1 person
Hi Kathi – I’m so envious of your homecare/outpatient programs (door-to-door transportation!?) It’s ironic that such excellence is somehow hamstrung by a failure to refer more heart patients to it before hospital discharge. Why should it be the responsibility of the visiting PT (you!) to educate your patients of the existence of outpatient rehab programs?
Also ironic that patients need to ask for homecare services. Thanks so much for your insights here, and good luck with your continued writing.
LikeLiked by 1 person
Great pondering here. Thanks again Carolyn for another insightful blog. My 2 cents is that changing the name could have the opposite effect, almost a sneaky little ploy to get those resistant to attend to participate just by ‘fluffing up’ the name.
We need to encourage patients that we understand we “just don’t feel like ourself” anymore. We are not to blame! This feeling is perfectly ‘normal’ as well as feelings of anxiety, PTSD and depression, etc.
I agree the priority is to get the referrals in the first place. I believe resistance can be from socio/ economic/ cultural reasons, as well as how our clinicians are ‘presenting’ their local Cardiac Rehab, both verbally & by their body language. Resources and empathy are needed, not a confusing name change.
Let’s use terms like ‘quality of life’ and ‘thriving’, not fear-based, like ‘do this and don’t do that in order to….’ Or even the word ‘surviving’.
As a coordinator of 2 ‘Support Networks’ for women with heart disease – often referred to as “support groups” – I personally recall a similar analogy. I was visiting another Support Group, and really felt the need to share some anxiety I was experiencing. Before discussion began, someone blurted out with a negative tone, “We need to change the name of this ‘support group’! We all sound like mental cases!”
You can bet none of us shares after that!
LikeLiked by 1 person
Steph, the more I read your comment, the more convinced I’m becoming that this whole name change question is a red herring. We need more heart patients to attend cardiac rehabilitation programs, so what can we do to make that happen? Let’s change the name!
Your ‘support network’ analogy is brilliant. Thanks for adding your voice here!
LikeLike
Carolyn, I will look forward to hearing more on this subject! I do think it’s all in the “presentation,” not the name.
LikeLiked by 1 person
As a society, we’ve become toooooooooooooo sensitive to words. I have grown tired of “political correctness” and giving words the credit or blame for people’s actions and decisions.
Rehab is is what the human psyche, not just the body, needs.
LikeLiked by 1 person
Such a good point, Judy-Judith. It’s the physicians who are failing to refer their eligible heart patients to cardiac rehab who need changing – not the name of the program they’re ignoring.
LikeLiked by 1 person
My Sudden Cardiac Arrest (my first heart symptom) did not qualify me for Cardiac Rehab.
I couldn’t believe it! I was DEAD, for crying out loud, I don’t know how much more needy I can be! Fortunately, I had a doctor who heard me when I described the crippling anxiety I now had about doing ANYTHING, including leaving the house. I couldn’t drive for 6 months, so that was a tiny bump in the road. I didn’t get to the point of being able to exercise with confidence, as my heart rhythms are still messy, but I did get educated, and grew in my confidence to be out among others in the world.
Perhaps the name “Cardiac Continuing Care” would make it feel more like a transition from this cardiac trauma that you’ve endured to the real life you need to live in and be functional. Although, “Cardiac Miracle” is also accurate, as they truly work miracles there!
LikeLiked by 1 person
I like both of your alternative names, Amy! My experience was certainly “miraculous”! Yet I’m still wondering if we’re focusing on right answers to the wrong question: is there any guarantee at all, for example, that changing the name of cardiac rehab will change the actual reality for patients who don’t/can’t attend, or for all those physicians who are failing to refer all eligible patients?
LikeLike
Great article! But frankly, I think having negative feelings about the name of cardiac rehab is pretty silly. It didn’t even cross my mind!
I knew I needed to be rehabilitated and I was grateful there was a program that could help me do it. I think anyone who would be embarrassed to go to “cardiac rehab” is just looking for an excuse to not go. I guess what other people “think” is just not that important to me… and I understand we don’t all think alike… but we’re talking life-and-death here!
Cardiac rehab saved me! I had been in rehab for six weeks before I could start cardiac rehab… just to be able to walk again. Then cardiac rehab took over and helped me regain my confidence and strength. It was also during that time that my Ejection Fraction went from 30% to 45%! And I’m sure that would not have happened without cardiac rehab. Also, I had so many questions, and my therapist was able to answer them all for me. It was a true lifeline for me!
As for why more people aren’t taking advantage of cardiac rehab – I would say that after reading this article and hearing a few comments in my group, I think the blame lies squarely with the doctors.
And when you read the statistics on how much cardiac rehab helps people – shame on them for not referring people to it!
LikeLiked by 2 people
Thanks so much for sharing your perspective here, Bonnie. My very small and unofficial survey certainly showed that the majority of women responding do agree with you – it is what it is, no need to change the name, basically.
But as the woman who left the 7th comment said very clearly (above), the negative association does exist for some (“she’s in rehab!” certainly has that celebrity headline-making familiarity to many people!) and yet she DID participate in cardiac rehab despite that negative deterrence, to her credit.
Cardiologist Dr. Gina Lundberg herself suggests the name should be changed. She is such an enthusiastic proponent of the program that I believe she’s simply trying to reduce every possible reason for NOT doing it. But is changing the name the magic solution?
Thanks also for pointing out what needs to be said: SHAME on the doctors who are not referring all of their eligible heart patients!
LikeLike
Reblogged this on Heart Matters and commented:
“I wasn’t offered cardiac rehab. As a relatively athletic person, rehab is a familiar term. Knee rehab is something that I’ve done after multiple surgeries. Given the numbers and importance of cardiac rehab, it’s shocking that so many doctors don’t recommend it.”
LikeLiked by 1 person
Thanks for sharing this post!
LikeLike
I participated in cardiac rehab with each of my two heart attacks. Four years later, I do my cardiac workout three times/week in the cardiac maintenance program. Cardiac maintenance is the post-graduate program to cardiac rehab. For me, it’s comforting to know that if I bonk while pushing the limits, then I am next door to the heart cath facility. I cannot compete after the heart attacks, but I do train for upcoming stress tests by running the Bruce protocol. And my cheerleaders – my fellow cardiac survivors – provide the encouragement!
For the new cardiac survivors, they are encouraged to work out with cardiac survivors who look and feel great. It’s a huge boost to their confidence. It’s where they can grieve with people who understand how they feel and they are accepted. It’s their safe place.
A lot of people stop attending, mostly those who cannot make time to train. They will be back….maybe, if they are lucky. Others cannot commit to lifestyle changes made necessary by losing the privilege of cardiac health. These folks really cannot accept that their body needs them to make changes – and they continue to smoke, drink, eat poorly, don’t sleep. They feel terrible and it’s pure misery to train when they feel so bad.
Others simply cannot afford the $30/month fee and pledge to continue at home on their own. One patient has recently lost her husband and her home/life is in disrepair. It’s pretty tough to have a heart attack on top of the life drama, and then add cardiac rehab to the existing time and money limitations.
My neighbor had a heart attack and I asked him when he was going to start cardiac rehab. He didn’t know about the program. We have the same internist so I questioned him as to why my neighbor didn’t know about cardiac rehab. The internist told me that he would – a GREAT idea and thanks for the suggestion…but nothing happened. I suspect that my neighbor asked if cardiac rehab would change any of his multiple medical conditions and the good doc admitted to the negative. When one is unwell in many areas, maybe they are just living out their life as they so choose?
A year ago, one of the survivors showed up after a long absence and explained that he came back because he wasn’t feeling well. I told him that he needed to go to the ER – that day – to get checked out. Really laid on the guilt/encouragement. He did and they caught the blockage before the heart was damaged. He lived and thanked me for saving his life.
I also see a vast number of people with terrible physical limitations – limited range of motion, weakness, muscle imbalances. These people need physical therapy to help them enjoy physical activities. Why is it that these wonderful people are not being referred into physical therapy?
Retirement makes it easy for me. I do my cardiac training 3 x per week at the hospital and strength/agility training 5x per week under an athletic performance trainer.
Other than that, the world is my gym – biking, hiking, gardening, reading and sleeping. I feel like a kid on summer vacation.
LikeLiked by 1 person
Love your last sentence, Anne – “Like a kid on summer vacation” – a great description of all that physical activity! That’s a good description of what cardiac rehab program prepares us for. Keep up the great work you’re doing.
LikeLike
My neighbor was told by both the doc and myself. He just wanted no part of exercise.
LikeLike
We have an excellent facility, here in Winnipeg, Manitoba, called the Reh-fit Centre, and I was immediately referred to their cardiac rehabilitation program by my hospital cardiologist when I was discharged from hospital two and a half years ago.
I did, however, run into a strong objection from my GP, when she heard about it. To be fair to her, she was not opposed to the program per se, but rather to its timing. Since I was left with a blood clot in the left ventricle after a serious heart attack, the so-called “widow maker” (one stent; one other 70% blockage left alone), and was at that point on three blood thinners – Coumadin (warfarin), Plavix and low dose aspirin – plus other drugs, after discharge, she felt it was too soon to begin an exercise program.
She feared vigorous exercise could provoke a stroke – walking was OK; exercise (weights, etc.) could wait until later. In the end, I never did go to “rehab”, relying instead on gradually longer and brisker walking with my husband as coach – he was an athlete in his youth, often injured, and knew that “slow and easy” would eventually get it done.
Like you, I was desperately weak and afraid, when I began walking and couldn’t go very far, but eventually improved. Now we walk briskly six days out of seven for 35 minutes/day (about 2 miles) without experiencing any angina pain or shortness of breath – and he still comes with me.
(I realise I’m very lucky – the blood clot has since disappeared and the blood thinners have been reduced to just the low dose aspirin.) One question: Is it true that once heart muscle is lost, it can never be regained? And if so, what is the point/goal of a rehab program, apart from restoring one’s confidence and general level of fitness?
P.S. I have no objection personally to the term in question, but “therapy” also appeals to me.
LikeLiked by 1 person
Thanks so much, Judy. I’m guessing that the “vigorous exercise” your GP was afraid of would not likely be what your Winnipeg cardiac rehab facility provides for any freshly-diagnosed heart patient. Sounds like your GP may have envisioned you roaring away on the eliptical trainer… In reality, as I observed in my own rehab, some heart patients were walking so slowly on the treadmill at first, that it seemed they were barely moving. That’s the beauty of supervised programs tailored to safely accommodate each patient’s unique condition. Some research, in fact, suggests that supervised exercise is more useful when initiated earlier rather than later – even for people living with heart failure.
Re the lost heart muscle: as quoted in this blog post, “The heart is not rehabbed by the exercise, but it improves the overall functioning of the body.”
Meanwhile, you and your hubby are doing great with your regular walking – keep it up!
LikeLike
I don’t have a problem with the name “cardiac rehab,” nor do I think it’s a misnomer. Interestingly, though, if you are in stroke or surgical recovery, you are often referred to “therapy”–speech therapy, occupational therapy, physical therapy and so on. So why in the particular case of the heart, did the powers that be decide to call the program “rehab” instead? No clue. (And do physical therapy patients worry that people will think they’re in therapy with a shrink? I doubt it.)
As I think about it, it seems that “rehab” may be more of a patient participant word, more active than passive — and I think that’s a good thing.
My bigger concern about what you’ve written, is that many cardiologists themselves do not appear to be aware of the substantial benefit of cardiac rehab.
As far as I’m concerned, therein lies the bigger problem. I suspect patients who want to improve their survival rates (and that would be most of us) would be happy to go along with any program that our doctors strongly encouraged. That many doctors don’t do this is appalling given the scientific evidence as to the benefits.
LikeLiked by 1 person
You are so right, Penny! As one of my readers wrote recently: “If doctors aren’t ‘prescribing’ cardiac rehab for those who need it, how would the patient ever know about it?” FYI, on March 29th, I’ve scheduled another blog post on this very topic: women’s stories of being referred to cardiac rehab – or NOT being referred and having to fight their doctors to get a referral. It is indeed an appalling reality.
LikeLike
I’m surprised patients aren’t doing rehab. I know that after my bypass and stent procedures, I was happy to do rehab as having someone monitoring you builds up the confidence to get back to a normal life…it lessens the anxiety of wondering how far you dare push yourself when you are finally doing it on your own.
LikeLiked by 1 person
Thanks Barb – that was 100% true in my own experience, too. Having a cardiac nurse right there watching and monitoring was the reassurance I needed to improve.
LikeLike