by Carolyn Thomas ♥ @HeartSisters
 Annette Pompa of Pennsylvania lives with a cardiac diagnosis I’d never even heard of until I, too, was diagnosed with it several months after surviving a heart attack. It’s called Coronary Microvascular Disease (MVD) or Small Vessel Disease. Unlike the classic Hollywood Heart Attack I’d initially experienced – which is typically caused by a significantly blocked major coronary artery – those of us diagnosed with MVD or coronary spasm disorders have few if any detectable blockages obstructing flow in the major blood vessels feeding the heart muscle. Yet we can experience the same distressing symptoms of a heart attack. Annette is a former art teacher who was barely 41 years old when MVD “came barging into my life”, as she explains. With her permission, I’m reprinting this transcript of an American Heart Association presentation that Annette gave recently about living with a non-obstructive heart condition.
Annette Pompa of Pennsylvania lives with a cardiac diagnosis I’d never even heard of until I, too, was diagnosed with it several months after surviving a heart attack. It’s called Coronary Microvascular Disease (MVD) or Small Vessel Disease. Unlike the classic Hollywood Heart Attack I’d initially experienced – which is typically caused by a significantly blocked major coronary artery – those of us diagnosed with MVD or coronary spasm disorders have few if any detectable blockages obstructing flow in the major blood vessels feeding the heart muscle. Yet we can experience the same distressing symptoms of a heart attack. Annette is a former art teacher who was barely 41 years old when MVD “came barging into my life”, as she explains. With her permission, I’m reprinting this transcript of an American Heart Association presentation that Annette gave recently about living with a non-obstructive heart condition.
♥
“This is my story. I represent an often misunderstood population living with a very different type of heart disease. Sadly, there are many more like me with MVD who are simply not being recognized – and indeed even dismissed. Symptoms often persist even without any visible blockage or reason for the angina, shortness of breath and fatigue which often accompany the condition. It is crazy, right? Here I was seemingly healthy – yet ended up battling heart disease.
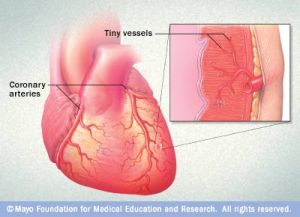 “What this means is that my tiniest of coronary blood vessels do not work well. And our smallest vessels are amazingly intricate. They feed the very heart muscle itself. The micro vessels make up 75% of the regulation for flow resistance within the heart. With mine being dysfunctional, my heart was starving for nutrients. It was not working well.
“What this means is that my tiniest of coronary blood vessels do not work well. And our smallest vessels are amazingly intricate. They feed the very heart muscle itself. The micro vessels make up 75% of the regulation for flow resistance within the heart. With mine being dysfunctional, my heart was starving for nutrients. It was not working well.
“Symptoms often persist even without seeing any blockage or reason for the angina, shortness of breath and fatigue which often accompany heart disease. Patients are then put through checking off the boxes of other possibilities, believing it simply can’t be the heart if there is not a blocked artery.
“I first started on amino acid supplements, hoping to boost my own natural nitric oxide production. But it wasn’t enough. Then I started trying various nitrates and incredibly, I found the level of nitroglycerin I needed. This can vary among Coronary Microvascular patients. I need what’s known as donor nitro – and not just small amounts here or there, but transdermal patches of it in varying amounts to deliver a steady hourly flow to my system which it lacks. For breakthrough angina pain, I also take Nitrostat sublingual tabs taken as needed (tablets that dissolve under the tongue). It is more than an average heart patient takes, but makes a difference in my symptom management. My blood pressure returned to normal and I could begin managing more time out of bed.
“But MVD means I am no longer able to hold a job, and I now focus on my best care and advocating for all people with non-obstructive heart disease issues.
“These small microvessels are affected sporadically all over my heart; physicians do not know why this occurs. That is another reason why it is hard to detect. There is no cure, but there are treatment attempts to manage my symptoms and keep those pesky micro vessels open! It is not considered as benign as it once was, and can cause truly slow and steady damage at the micro level, especially if ignored. It’s a heart condition that needs prompt care and respect to give patients their best quality of life dealing with this chronic condition.
“Here is something interesting: when patients seek help for cardiovascular symptoms, over half of them are found to have non-obstructive heart disease. 60% of women with symptoms of heart disease learn during an angiogram that they do NOT have visible obstructions in their coronary arteries despite their serious cardiac symptoms.
“Coronary Microvascular Disease is difficult to diagnose and treat. There are roughly 90,000 new cases a year.
“Chronic angina significantly impacts quality of life, ability to work, and costs to society [1].”
“85.6 million in the US are living with heart disease or the after-effects of stroke. That is an incredible number. Now think about it. We often focus on the 80% of that number – heart disease that can often be prevented. We must strive to change all we can. If we can do something to protect our precious engine, then that is what we should do. Be informed and proactive.
“However, being able to avoid this number one killer is not always possible.
“With heart disease rates not decreasing AND more areas misunderstood, we need more research. We need widespread clinical understanding for our local doctors to see that there is a percentage of people often being dismissed and lacking immediate important care.
“Supporting research on MVD could help reverse these sad numbers of people who are attacked by an often unseen killer. It may even help change the way statistics are heading. The numbers are growing in heart failure that’s linked with non-obstructive cardiac conditions. Patients living with heart failure – but with “normal” ejection fraction – are expected to be the overwhelming majority in the future. Why? We are getting rather good at intervening when it is possible. Bravo! Yet we have a long way to go to understanding the often unseen, sneaky non-obstructive issues.
“Here’s how to protect yourself:
- You must trust your body and its symptoms, and respect what it is telling you.
- You must find patient-centered care and be persistent.
- Be your own advocate and learn all you can about living a healthy life to be your best.
- Control what cardiac risk factors you can control.
- Be on the lookout for new developments.
- Advocate and search for better ways to beat heart disease, our #1 killer.
“We can work towards reversing these mortality numbers. We can and must work towards a better heart health future for us all.”
Image: ©Mayo Clinic
♥
© 2016 Annette Pompa
[1] Excerpt From: Juan Carlos Kaski, Guy D. Eslick and C. Noel Bairey Merz. “Chest Pain with Normal Coronary Arteries.” Springer London, London. 2013
Q: Were you aware of coronary microvascular disease before reading Annette’s story?
Learn more about Coronary Microvascular Disease and other non-obstructive forms of heart conditions:
UPDATE November 2019: Diagnostic tools used to identify coronary microvascular dysfunction
More from the WISE study (Women’s Ischemia Syndrome Evaluation). This research from the National Institutes of Health began in 1996 to increase scientific knowledge about ischemic heart disease in women.
♥ You can watch videos of the 2019 INOCA International “Meeting of the Minds” cardiology conference in London, including Dr. Juan-Carlos Kaski’s presentation on microvascular disease.
Could You Wait 10 Years for a Cardiac Diagnosis? (Bobbi-Jo Green’s 10-year fight for an accurate diagnosis of non-obstructive heart disease
Coronary Microvascular Disease: a “trash basket” diagnosis?
Misdiagnosed: Women’s Coronary Microvascular and Spasm Pain (how to diagnose non-obstructive heart disease)
My Love-Hate Relationship with my Little Black Box (how a non-invasive, non-drug therapy has affected my own MVD symptoms)
How Women Can Have Heart Attacks Without Having Any Blocked Arteries
Small Vessel or Coronary Microvascular Disease – from Mayo Clinic
A Cardiologist’s Advice on How to Use this “Wonder Drug” (on taking nitroglycerin to relieve angina pain)
Watch this 5-minute video about Joan Jahnke of South Carolina who went to Emory Heart & Vascular Center to have her MVD appropriately diagnosed and treated
“I Rang the Bell Again. No One Came.” An Australian woman’s shocking account of being dismissed by hospital staff even when she carried with her a letter from her cardiologist explaining her twin non-obstructive heart conditions of MVD and Prinzmetal’s Variant Angina.
.
NOTE FROM CAROLYN: In my book, “A Woman’s Guide to Living with Heart Disease“ (Johns Hopkins University Press), I included much more about how all forms of women’s heart disease can differ from men’s in research, diagnostic accuracy, treatments and outcomes. You can ask for this book at your local library or favourite independent bookshop, or order it online (paperback, hardcover or e-book) at Amazon – or order it directly from Johns Hopkins University Press (use their code HTWN to save 30% off the list price).

Your article hit home. I am an RN who has been dealing with the symptoms for over a year. I cannot find a doctor with any expertise on MVD. The only symptom I have not mentioned in your article is chest pain and tightness in cold air and strenuous exercise..I have failed with channel blockers. I am now trying low dose nitro patch.I would appreciate any recommendations for cardiac physicians in the Rochester or Syracuse area who specialize in MVD.
LikeLiked by 1 person
Hi Tonya – I’m sorry to hear of your symptoms, and also your inability to find a physician who is informed about MVD. I too experience MVD chest pain in the cold – even walking down the frozen food aisle can set me off. I live on the west coast of Canada and am not familiar with cardiologists in New York State, but I suggest you do a Facebook search for an MVD patient group started by Annette Pompa called “Heart Whisperers”. I’m sure one of the 600+ women on this group might be able to steer you in the right direction.
LikeLike
Hi! I am a 50 year old mom of three. We are presently residing in Saudi Arabia. Three weeks ago I was taken to the ER due to chest pain and shortness of breath. I did the necessary tests: ECG, x ray, 2D echo, troponin and all are normal. I did a stress test and there is an ST depression. I was diagnosed with positive myocardial ischemia. I did a CT Coronary Angiogram and based on preliminary findings, there are no narrowing or blocked arteries.
The official medical result is coming out after three days. I still have on & off chest pain, shortness of breath, abdominal pain going to my left side. I am taking aspirin, beta-blocker (Concur), clopidogrel, and statin for my cholesterol. I have no hypertension. I know that what I am experiencing is not “all in the mind”. I just wanted to share. Thank you.
LikeLiked by 1 person
Hello Suzette – I’m not a physician so cannot comment specifically on your situation except to say that a person showing diagnostic test results with an ST depression and ischemia is not having symptoms that are “all in the mind”. I hope that your official medical results will help your doctors determine the next step in addressing your symptoms. Best of luck to you…
LikeLike
Just read through all the comments and realising what a complex diagnosis it is. I wanted to reassure new nitro users that the headache does go away if you persevere. At xmas I could barely stand with the pain which felt as though somebody had my head in a wringer. It took three months to stabilise and my worst time was when I woke up. It is still around, but I have a morning routine I stick too. Wake up, two pain killers if the headache is pounding. Mug of tea and half an hour later a warm bath. The more I fought the pain the worse it was. Never a pleasant drug but if it alleviates my angina symptoms worth putting up with. I was told nitrates open up the arteries in your head as well – hence the pain.
LikeLiked by 1 person
Hi again Liz – you’re right, that’s how nitro works. Read more on taking nitro from pioneer cardiologist Dr. Bernard Lown.
LikeLike
Brilliant- at last a concise easily-read document about coronary microvascular disease. I am not alone thankfully, but I do have a few things to add which may be useful.
I was diagnosed Christmas 2016 due to an excellent cardiologist. I had an angiogram which showed I had a slightly smaller left anterior descending artery. However during the angiogram when the dye was inserted I experienced the same pain which took quite a while to get under control. During a discussion with my specialist he said that often people with this have a history of high blood pressure (I have had that for thirty years) and Type 2 diabetes (Diagnosed with that at thesame time).
Provided you can keep your sugars and your blood pressure under control that goes a long way to reducing further damage. I am using two heart drugs and a spray and since they have kicked in I only have a few mildish attacks.
The great thing for me was getting a diagnosis and knowing it was not in my head! As was said in the article so many get missed until a heart attack comes along! I am now back to normal – whatever normal is of course! I try not to worry about it, keep exercising gently and avoid too many carbs. Blood pressure is a bit more difficult as it is messing about at the moment. I am currently around 150/90 which my GP feels is too high given the BP drugs I am taking.
So welcome to fellow sufferers, but there is light at the end of the tunnel if you get diagnosed correctly!
LikeLiked by 1 person
You are correct, Liz. Many people with MVD apparently also have diabetes or high blood pressure. Also true that, without a correct diagnosis, there can be no effective treatment plan. Sounds like you are on the right track these days – keep up the great work!
LikeLike
I am glad I found this site. At age 40-41, I found out that I have chest pains when I run. I went to so many doctors, so many invasive tests but they found nothing wrong with my heart. So finally someone said this is Syndrome X. I stopped going to the doctors. The good news is that my heart does not hurt me unless I walk uphill, upstairs or run. Otherwise no problem. Now I found out here that I have MVD, it makes sense. I will go see a cardiologist again and discuss course of action if any. Thank you all for sharing your case and knowledge.
Alexandra
LikeLiked by 1 person
Hello Alexandra – best of luck to you at your return visit to your cardiologist.
LikeLike
I have just been diagnosed with this thanks to my experiencing it while having an angiogram and an excellent cardiologist who knew his stuff. Interestingly this can be linked to type 2 diabetes and I was diagnosed with that the same week.
The relief of having a diagnosis when I had experienced severe pain and been rushed to A and E only to be told I did not have heart problems, is immense. New tablets and now new hope I will get this controlled soon
LikeLiked by 1 person
Talk about good timing, Liz! Glad you were in the right place at the right time. Good luck to you in managing both diabetes and heart stuff…
LikeLike
Thanks Carolyn – onwards and upwards. Just spoken to a nurse friend of mine and she was unaware of this disease. I dreaded being told there was nothing wrong when I knew there was. Good old NHS in Britain got it right!
LikeLiked by 1 person
Unfortunately, some doctors are not as familiar as they should be with coronary microvascular disease. One of my blog readers, for example, after she had asked her physician if her distressing symptoms could be due to MVD, told me that he had replied: “I don’t believe in that diagnosis” – as if they were talking about the tooth fairy or Santa Claus! That’s pretty inexcusable…
LikeLike
Hi, my name is Annette. On November 2, out of the blue, right after my 45th birthday, my heart had pain, I had shortness of breath, dizziness, arm pain, jaw pain for 2 weeks, before I was admitted into the ER. 3 days of tests showed no damage and no blockages, the only thing off was the stress test- it was 7 minutes long, last year was 14. One cardiologist picked up on that and had a diagnosis of MVD; the other, who was my cardiologist and discharged me as muscle pain, told me to take a Motrin if I experience heart pain and shortness of breath!
I can’t concentrate. I have chest pain on and off, take Nitro’s, have shortness of breath, and I am so very tired. So tired all the time. I am otherwise healthy and skinny and have always been so active. I have a low blood pressure, always have. The Cardizem one doc prescribed lowers it even more, and I am more fatigued, but at least it’s something, until I can dive into this a bit more.
I am really interested in people’s opinions and help. And had I not pressed my own PCP to call upon the cardiologist that saw me and doing my own research before I went in to ER, I don’t think anyone would have really cared. I did not have a heart attack, but from the sounds of it, it seems if I don’t get it under control, it’s something that could come. My father and his siblings all have/had heart trouble early in life. Any advice to me, just starting this journey??? How to get people to listen??? And I have never, ever been one to complain…unless it was necessary. How do I get dr’s to understand that???
LikeLike
Hi Annette – I’m not a physician so cannot comment specifically on your symptoms, but I can say in general that right now, you don’t know if your symptoms are heart-related or not. Something however is causing them. If I were you, I’d request a medication review. Cardizem is a calcium channel blocker that works by relaxing the muscles of your heart and blood vessels, often used to treat chronic stable angina (chest pain) or coronary artery spasm. It sounds like it is not working for you (which also may hint at a non-cardiac cause). But as you correctly say, it’s also used to treat high blood pressure – which you don’t have. A medication review will help your doctor assess a drug prescribed to do one thing (reduce your angina) but is making something else worse (low blood pressure). You need to find out if the drug itself is adding to your symptoms. If it’s not addressing your chest pain, and it’s making you feel weak, it’s time to reassess. You must discuss this with your prescribing doc (although you might be worried about being perceived as “difficult“, tell your doctor that this is a quality of life issue). Many of my readers tell me they suffer quietly despite ongoing symptoms, hoping that things will somehow magically get better on their own. Sometimes they do (!) but often this delay just means needless suffering. Please make an appointment. Good luck to you…
LikeLike
I am a Nurse Practitioner and am being worked up for possible ischemia ( heart disease) due to “Nonspecific T Wave Changes” on my EKG. Local cardiologist feels no further workup needed. I got a second opinion and am scheduled for a stress test and echocardiogram. The fact your stress test was abnormal is significant. Please take time to read about the WISE trial. It is a landmark study about women and heart disease. Women often have normal appearance of coronary arteries with angiogram testing. Experts feel women have Micro Vascular Dysfunction (MVD). Read and take notes about results of the WISE trial and discuss with a different cardiologist. WISE trial results show that Calcium Channel blockers do NOT help! (which includes your medication Cardizem). Consider referral to Cleveland Clinic or Mayo Clinic in Rochester, MN if you don’t live too far away.
Good Luck!
LikeLike
I was just told that I’m going to need an MRI from head to toe because my doctor heard a blockage in my left side growing in my artery. I’m just terrified because of what I saw my mother go through before she died. Please Carolyn can you tell me what can I expect will happen?
Thank you.
LikeLike
Hi Marianne, I’m not a physician so cannot comment specifically on your case. I’m not sure, for example, why you would be recommended a full body MRI rather than a cardiac MRI to examine only the heart. I’m guessing you have been having symptoms (which is why an MRI would be recommended) but again, I’m not a doctor. There are a number of comprehensive sites that help to explain what to expect during an MRI procedure far better than I could, for example Mayo Clinic or Cleveland Clinic. So do some thorough homework and try to avoid feeling “terrified” in advance – these are just tests, and they will help your doctor to help you.
Best of luck to you…
LikeLike
I really needed to read your article today. I was admited to hospital last year with what was first diagnosed as a mild heart attack and then later changed to Prinzmetal’s angina as my arteries were clear.
I am still not feeling well and have a second cardiologist who is not sure it is Prinzmetal’s angina. My blood tests in emergency showed the heart issues but the dye test showed everything well. It’s so frustrating as I still have chest pain and use nitrates, but I do not know how to prevent or what is causing this. I have continued to work and have just been put off on sick leave. I sometimes can barely walk to my car due to shortness of breath and fatigue. I always had tons of energy but this has changed since last year. I currently have a heart monitor but of course no episodes, and I am not sure it would show anything. I know it’s not anxiety but now yes I do have anxiety over this. I hate taking the nitrate due to headaches but it does make me feel better besides the side effects. I will read more on your site.
Thank you and this is going to make me more persistent as I know I am not well and I feel dismissed. I just want to know what is going on.
Lisa
LikeLiked by 1 person
Hi Lisa – I’m not a physician so of course cannot comment specifically on your symptoms or diagnosis, but I can tell you in general that you’ve hit upon a very common reality: there are few things in life more anxiety-producing than having scary bouts of cardiac symptoms, especially if you don’t have a clear and definitive diagnosis. No wonder you feel anxious! Read this about taking nitroglycerin – it may be hard for you to believe this now, but the famous nitro headache usually does get better over time (with some exceptions, e.g. people who already have a long history of migraines).
But having said that, I remember vividly in the early days holding my nitro spray and wondering which was worse: this chest pain or the nitro headache I’m about to feel if I use this spray?!? Try taking a Tylenol about 15 minutes before your nitro – many of us find that this often does the trick to help minimize the headache side effect. I rarely if ever notice a nitro headache these days, and I use it several times a week. You might also want to check out the WomenHeart online support community’s topic on non-obstructive heart disease. Hang in there, Lisa!
LikeLike
Hello Carolyn,
Thank you for your eye-opener article. It so happens that not only myself but also my 41 year old daughter who just had her first “scare” and is still in the midst of finding her diagnosis have had cardiac symptoms. I personally had a “type 2” heart attack in June 2015. After two angiograms and no blockages found, cardiologists suspect MVD although my diagnosis is not conclusive as of yet, a year later.
The reason for this comment is: I was prescribed nitrogen oral form but it gives me unbearable headaches and I’m wondering now if any other form or via other than orally might work for me. I was not aware of nitro derma patches or sprays. Would it give me the same side effects? I’m willing to look into it if that’s a key to a more “normal” life”. Thanks again and best of luck…
Marie A.
LikeLiked by 1 person
Hi Marie – that must be very stressful to have your daughter now experiencing what seems like cardiac symptoms, too. My understanding is that all forms of nitro have the famous “nitro headache” as a possible side effect, particularly if you’re a person with a history of severe migraines. That’s how the drug works: it’s a “vasodilator” and that means dilating the blood vessels to the head/brain as well as to the heart. Long-acting nitro (in pills or patch) tend to produce fewer/less severe headaches after your body adapts. But not every heart patient should use long-acting nitro (generally it’s only appropriate if you have more frequent angina episodes. Ask your doctor about this option).
Meanwhile, remember to take a Tylenol before your dose of nitro: the painkiller might outrun that nitro effect. Also, read this post featuring Dr. Bernard Lown’s take on nitroglycerin; he calls it a “wonder drug”.
LikeLike
I have had a growing list of heart trouble symptoms for 30 years. Started out as light, infrequent chest pain, then palpitations, left arm pain, inability to do strenuous things, some shortness of breath, etc. Symptoms have slowly built in intensity and frequency. A week ago I went to a cardiologist who said it can’t be my heart because you can’t have symptoms for 30 years and have it be your heart. Has anyone else had very long-term, slowly growing symptoms that indeed ended up being heart trouble?
LikeLike
Hello, Kari,
I’m not a physician so of course cannot comment specifically on your symptoms. But I can say generally that 30 years is too long to be living with increasingly debilitating undiagnosed symptoms, whether they are heart-related or not. And it is also possible to be living with stable angina (chest pain/shortness of breath/other symptoms that typically come on with exertion and go away with rest) for years. (I personally know of several people like this, including one heart patient I met at Mayo who loved playing tennis despite her chronic stable angina. She stops halfway through each daily tennis game to sit down, have a dose of nitroglycerin spray for angina pain, wait five minutes, and then continue happily with her game; she’s been living like this for many years). Try keeping a symptom journal to show to your physician (noting if your symptoms become worse when associated with exertion, emotional stress, eating a heavy meal, smoking, etc.) Something is causing your symptoms; right now you just don’t know if they are heart-related. Best of luck to you…
LikeLike
NOTE FROM CAROLYN: This comment has been deleted because it pretends to be from a patient while (very poorly) disguising its link to a cardiology practice in India soliciting new customers.
LikeLike
This article was so informative. I’ve lived with this for 20 years, and been through all the misdiagnoses of anxiety, panic attacks and gastro. Four years ago my internist told me the cardiac tests were normal, and I just needed to get over this and get on with my life. Needless to say, I changed doctors. I now have a supportive and informed cardiologist and primary care doctor.
This is real, it does affect my life, and I am now my own best (and informed) advocate when the angina gets out of control. Educating oneself and others is necessary.
Thank you for your story.
LikeLiked by 1 person
Hi Laura – a physician who tells you that you just need to get over this and get on with your life is somebody who doesn’t have answers, so blames the person asking the question. So glad you finally found your current medical team!
LikeLike
I do have a great team now, and have learned to take the good days and enjoy them. On those days when the symptoms are worse, I’ve learned not to stress, but to accept what it is, what I need to do, and seek further help when necessary. So glad to see this condition being recognized and further research being conducted.
LikeLiked by 1 person
Laura, if you haven’t already read it, check out this post on using TENS therapy (a non-invasive, non-drug treatment for the refractory angina of coronary microvascular disease). I’ve been clipping my little TENS unit onto my belt every morning for the past seven years to address my own MVD angina since both my cardiologist and pain specialist recommended this for me seven years ago. Since 2001, the U.K. National Refractory Angina Centre has in fact recommended neuromodulation therapy of TENS for persistent angina in heart patients, e.g:
“Neuromodulation should be offered as part of a multidisciplinary angina management program based on the current guidelines.“
LikeLike
Subscribing to HeartSisters changed my life, but this article describing Annette Pompa’s Coronary Microvascular Disease…I BELIEVE…may change my HEART.
I have done so much research and I’ve glossed over this SO many times, and ironically, I received a diagnosis of “Mild Non-obstructive Coronary Artery Disease” because my Left Anterior Descending coronary artery was found to have a 30% occlusion, and also I was confirmed to have had an non-STEMI heart attack when I presented in the ER that weekend with shortness of breath and chest pain.
So angiogram pre- and post-diagnosis they kept as nSTEMI, with the other listed in the report about the arteries, with nothing about small arteries, including stenosis. Interestingly, my 4-day inpatient stay Admission Diagnosis was “Anxiety and Dehydration” and my discharge diagnosis was “Anxiety and renal insufficiency”. I’m thinking about having this amended after reading your enlightening and valuable life-saving article about Women’s Heart Attacks and Panic Attacks compromising women’s overall Cardiac Healthcare.
I now feel that there is a huge chance that my ongoing sometimes severe (and to my cardiac team, unexplained) angina, shortness of breath, blood pressure swings, and the fact that I can no longer hold my teaching career lead me to believe that I may have Annette Pompa’s type of Coronary Microvascular Disease. I’m already doing the Nitro Spray and Imdur, but if a patch could help, then I’m making an appointment.
Again, HeartSisters is INVALUABLE to me and thank you for this article. Between the ANXIETY piece and this, I believe I am connecting the dots to my severe symptoms that doctors shrug their shoulders to. Thank you so much, before this article, it was in my face…but I really did not know about Coronary Microvascular Disease. Please don’t ever STOP this work!!!!
LikeLike
Thank you for your kind words about my site, Patricia. I’m not a physician so of course cannot comment specifically on your symptoms, but getting a second opinion is certainly a good option. There are only a few specific cardiac tests that work for diagnosing coronary microvascular disease – the standard angiogram typically used to identify large blockages in large arteries (as you have already had) can’t pick up MVD like, for example, the test called coronary reactivity testing (see more about diagnostics here). Whatever your diagnosis, symptoms that are bad enough to make us unable to work should be addressed, and yes, they can be debilitating enough to make us anxious, too. Best of luck to you…
LikeLike
It is so important to share this information. At 47 I had an Atrial Myxoma removed. I had no idea that they existed. Thank goodness one doctor (after seeing many) understood that something was wrong and identified the problem.
This website is so important for women and their families! All the best to you!
LikeLiked by 1 person
Thank you for your kind words. (Readers, FYI: an Atrial Myxoma is a tumour in the upper part of the heart). Luckily, your doctor identified it correctly!
LikeLike
It is really good to hear about more cases of Microvascular angina being recognised and treated. My first angiogram showed severely blocked arteries so immediate bypass surgery was the obvious treatment and this should have cured all my angina symptoms.
But as it didn’t, I had to take the slower path to a confirmed diagnosis and effective treatment for my Microvascular angina. Nitrates in higher doses (smaller doses were perhaps misleadingly ineffective) have proved to be the most effective part of my medication. I now take daily 100mg of a long acting mononitrate and I have GTN slow release patches for when I want to be extra active. I have GTN spray as a reliever if I have temporarily overdone it and get chest pain. I used to get longer spasm attacks but not so far under this treatment. Although I am not ‘cured’ or symptom free, it is so well controlled that I have been able to be more active and successfully improve my heart fitness.
Last year I was invited by the British Heart Foundation to tell my story as part of an article in their magazine ‘Heart Matters’: ‘All about Microvascular angina’ – based on an interview with Professor Juan Carlos Kaski and the link to my story – ‘Jennifer’s story of Microvascular angina‘.
Thank you for wonderful ‘Heart Sisters’ Carolyn, which I have been reading for years now!
LikeLiked by 1 person
Thanks so much for sharing that terrific British Heart Foundation article, Jennifer! So much of your story mirrors mine: I too had to quit working at about the same age because of my MVD symptoms, and I too find that regular daily exercise (and of course my nitro!) really help me to function. It’s so important to spread the word that not all heart conditions involve big blockages in big coronary arteries. Many people with ongoing cardiac issues like ours are dismissed or simply told “It’s not your heart”. A few years ago, I included a link to a short video about Professor Kaski’s work in this post. Thank you again for sharing your experience with us!
LikeLike
I have been diagnosed with small vessel disease after 2 stents, one in 2010 and one in 2013. I have had chronic angina since the last stent. Then my cardiologist told me I had small vessel disease. That’s what he called it. I have not felt right for a very long time especially this last winter. It was terrible until at the end of May I found a website called http://inclinedbedtherapy.com/. I read it and my husband and I decided to try it because he snored so bad. So we raised the head of the bed 6 1/2 inches. The difference in the way I felt was immediate. I had energy and no pain. I felt normal again. I have had one episode of angina since then where I had to take nitro. But it surely has helped me!
LikeLiked by 1 person
Wow, that’s amazing, Mary Kay. You might also be interested in reading Dr. Steven Park’s work on sleep breathing disorders (which he warns are closely linked with cardiac issues). BTW, did adjusting the bed also fix your hubby’s snoring?
LikeLike
It helped my husband a lot. Not all the way – but nothing like it was!!
LikeLiked by 1 person
Hurray (for both of you!)
LikeLike
I also have arterial spasms and just finished 35 EECP treatments for chronic angina. I was hoping I would be pain free now, but it is not so. I believe the treatments are of value however. I learned to use nitro more often, and I am now much more active and focusing on that. I hope this over time will make a difference for my spasms, as well as helping general heart health. The spasms have made me lazy and afraid of pain and that is not the way to go! Ranexa used to help but I have to take so much now, I struggle with side effects. Will try nitro patch. Thanks! And I am also exploring the life choices that have given me a “broken heart”. I think its all part of it!
Love the website and feel heard. Thank you.
LikeLiked by 1 person
Lian, thanks so much for sharing your experience here. I sure can identify with your sense that a fear of pain can indeed change one’s personality (and level of activity!) Good luck with that nitro patch – I like to remind myself that “nitro is my friend!“
LikeLike