by Carolyn Thomas ♥ @HeartSisters
 Dr. Jennifer Co-Vu is a pediatric cardiologist at the University of Florida Congenital Heart Center. She recently shared on Twitter a chilling report of what happened when 911 was called to help her own mother-in-law who was experiencing crushing chest pain. The ambulance arrived quickly, but paramedics told this 65-year old woman with diabetes that she was having a panic attack.
Dr. Jennifer Co-Vu is a pediatric cardiologist at the University of Florida Congenital Heart Center. She recently shared on Twitter a chilling report of what happened when 911 was called to help her own mother-in-law who was experiencing crushing chest pain. The ambulance arrived quickly, but paramedics told this 65-year old woman with diabetes that she was having a panic attack.
Unlike other women who are misdiagnosed in mid-heart attack, however, this patient had immediate access to something few of us have: doctors in her family. ..
Worried that this scenario sounded far more serious than a panic attack, her husband called their son (Dr. Co-Vu’s husband, who is also a physician) and asked him to intervene.
At first, the paramedic insisted to the son that his mother was not having a heart attack. He also recommended anti-anxiety medication.
Dr. Co-Vu describes her husband’s role in this intervention with the paramedic as “begging nicely”, adding:
“I wouldn’t have been as nice, and would have asked the paramedic if he had already given her aspirin, and then told him that I’m going to start timing his response to ‘door to balloon’ time.”*
The paramedic was ultimately persuaded to change his mind, and decided to take the woman to Emergency after all, where her heart attack was correctly diagnosed and treated.
But as Dr. Co-Vu observed:
“The real reason for disproportionately poor cardiac outcomes in women is NOT how chest pain is described, but how women’s chest pain is perceived. We need to refocus education to include the front line.”
She also added this about her mother-in-law’s experience:

Good question, Dr. Co-Vu.
Do we really need to beg?
The disturbing answer is that we might need to beg if the person having alarming cardiac symptoms is a woman. See list of related published journal links below for specific examples…
As Dr. Co-Vu says, it seems “surprising” that any paramedic’s initial diagnosis of a person with known cardiac risk factors and Hollywood Heart Attack symptoms like crushing chest pain would be “panic attack“.
But I’ve heard far too many similar stories from my readers over the past decade to be surprised by almost anything anymore.
There was something else about this story that bothered me almost as much as the misdiagnosis: Dr. Co-Vu’s mother-in-law was taken to Emergency only because her son-the-doctor intervened on her behalf.
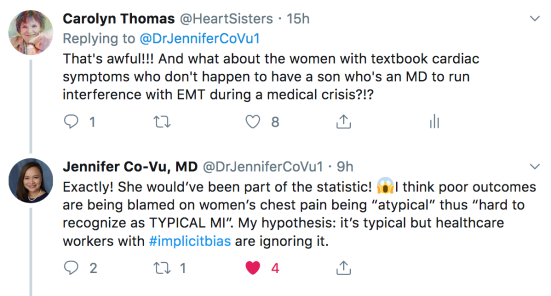
I shared this concern on Twitter with Dr. Co-Vu:
The implicit bias that Dr. Co-Vu is now personally acquainted with since her own family member’s alarming experience is alive and well in cardiology.
Researchers continue to report that female heart patients tend to be under-diagnosed (and worse, under-treated even when appropriately diagnosed compared to our male counterparts) in what’s become known as the cardiology gender gap. See also: Excuse me while I bang my head against this wall…
Our resulting poorer outcomes compared to men are often blamed on this implicit bias against women among medical professionals.
As you already know if you’ve read the disturbing results of many emerging studies that I’ve written about (here and here, for example), researchers who study this phenomenon compare how male heart patients are treated when compared to their female counterparts. See also: Cardiac gender bias: we need less TALK and more WALK
One of the most disturbing recent examples was a study published in 2018 in the journal, Women’s Health Issues.(1)
Researchers compared the pre-hospital care of both male and female heart patients over the age of 40 who had been transported to hospital after calling 911 for help.
It wasn’t only the study’s findings that women being transported to hospital were less likely than men to receive recommended treatments (including even the minimal basics such as aspirin or cardiac monitoring) that shocked me. That appalling reality has been reported by cardiac researchers so many times that’s it’s at risk of being considered tired old news by now (for example, Pope et al., 2000; Blomkalns et al., 2005; Jneid et al., 2008; Dey et al., 2009; Meizel et al., 2010; Balady et al., 2011; Poon et al., 2012; Koopman et al., 2013, etc. etc. etc.) See also: The Sad Reality of Women’s Heart Disease Hits Home
It’s also why we are often forced to conclude, in the wise words of Laura Haywood-Cory (who survived her own heart attack at age 40):
“Sucks to be female. Better luck next life!”
But the part of this study that seemed to cause the most excitement was this conclusion:
“When transporting female heart patients from the scene to the hospital, Emergency Medical Services (EMS) personnel were significantly less likely to use lights and sirens compared with male patients being transported.”

And as Dr. Co-Vu also determined in her Twitter exchange, the defense offered for women’s poor outcomes during a heart attack is often that women’s symptoms are “atypical”, thus easier to misdiagnose than in men. She now maintains that even clearly “typical” cardiac symptoms like the crushing chest pain suffered by her mother-in-law can be ignored by healthcare professionals due to this pervasive implicit bias against women.
Some of the same professionals may blame women’s poor cardiac outcomes on women themselves. Maybe, they suggest, our poor outcomes are due to women’s tendency to delay seeking emergency care, or because of the way we communicate our cardiac symptoms to physicians.
But instead of continuing to blame the female heart patient, why not expect the ones who are making decisions based on implicit bias against women to wake up?
Women should not need to have two physicians in the family in order to get appropriate care during a cardiac event.
♥
Image of begging frog from Alexas/Pixabay
* Door-to-balloon (D2B) time: The time between the arrival at a hospital of a patient with an acute heart attack and the opening of that patient’s blocked coronary artery via balloon angioplasty (and usually a stent). The recommended D2B time is 90 minutes or less for best outcomes.
1. Lewis, Jannet F. et al. “Gender Differences in the Quality of EMS Care Nationwide for Chest Pain and Out-of-Hospital Cardiac Arrest.” Women’s Health Issues, December 10, 2018.
NOTE FROM CAROLYN:I wrote much more about identifying cardiac symptoms (even if you don’t have a doctor in the family) in Chapter 1 of my book, “A Woman’s Guide to Living with Heart Disease”. You can ask for it at your local bookshop (my preference!) or order it online (paperback, hardcover or e-book) at Amazon, or order it directly from my publisher, Johns Hopkins University Press (use their code HTWN to save 30% off the list price).
♥
Q: Have you or a loved one ever felt like you had to beg for appropriate emergency treatment?
See also:
How can we get female heart patients past ER gatekeepers?
Fewer lights/sirens when a woman heart patient is in the ambulance
Excuse me while I bang my head against this wall…
Same heart attack, same misdiagnosis – but one big difference
Cardiac gender bias: we need less TALK and more WALK
Unconscious bias: why women don’t get the same care men do
Words matter when we describe our heart attack symptoms
‘Gaslighting’ – or, why women are just too darned emotional during their heart attacks
The heart patient’s chronic lament: “Excuse me. I’m sorry. I don’t mean to be a bother”
Heart attack misdiagnosis in women
The sad reality of women’s heart health hits home
Gender differences in heart attack treatment contribute to women’s higher death rates

Yes, as in my sister-in-law’s experience with the EMT who also diagnosed “panic attack.”
She replied “I’m going to die here!” And promptly did just that. Lights and siren didn’t go on until her vitals took a leap right during their exchange. Pitiful. And my poor niece witnessing this from the front seat.
LikeLiked by 1 person
Oh Pat!!! I am so sorry for your loss. What a tragic and horrible experience for your whole family to suffer. And her daughter sitting right there watching, helplessly. A nightmare…
Putting on lights and sirens only when her vitals looked bad somehow makes the story seem even worse. Recent research does suggest that lights and sirens are in fact used less often when the patient in the back is a woman (so that part of this dreadful experience may not be uncommon!), it sure smells like another horrific example of implicit bias at work. My condolences to you and your family…
LikeLike
Hello,
I’m not sure what the scope of practice for paramedics in Florida is but I’m thinking medical diagnosing is likely not part of it.
Deciding this was a panic attack without proper medical work up is a huge liability. Had this woman died, his company and possibly even himself personally would have left themselves wide open for suit.
It is truly incredible that with all the medical knowledge we have this common problem is still being treated this way, especially in women.
LikeLiked by 1 person
I agree 100%, Joanna! Somehow, I cannot even imagine, if that paramedic were responding to a MALE patient who was experiencing crushing chest pain, that “panic attack” would be the differential diagnosis…
First diagnosing (er, MISdiagnosing!) and then arguing with a physician trying to convince him you’re right – and he’s wrong! That requires a special kind of arrogance… Dr. Co-Vu did mention her intention to speak to the paramedic’s superiors – in order to use this experience as a teaching tool about the perils of “impicit bias” for all paramedics out in the field.
LikeLike
Boy, after reading this amazing and appalling story, my question was — what is the purpose of a paramedic?
I mean, I really do know the answer — but it seems to me that they should not be the ones to make the diagnosis. It should be their job as first responder to just assess and stabilize the patient’s condition, report to the hospital with possible diagnoses, and get the patient to the ER ASAP so doctors can make the final diagnosis. To ignore the factors presented here that made it more than reasonable to suspect a heart issue, even to not be willing to transport the patient to the hospital to rule out a heart issue — wow, he really overstepped his bounds there. That was just all wrong.
Wouldn’t it be better even just to err on the side of caution?
I did wonder why the parents didn’t call their cardiologist daughter-in-law instead, if the son wasn’t a cardiologist. And yeah, the son should have been a lot more firm with the paramedic, and I hope they reported this to his superiors.
The one time I called 911, when my heart went into a-fib, I was pretty positive I knew what it was, given that my husband has this too. We are both heart patients and I have 2 stents, and have been so drilled by the cardiologists I know that I should call 911 that I felt I had to do that.
The whole ambulance/911 experience was weird (and very expensive too). The people at our local small-town fire dept down the road from us were having a banquet (I found out later) so three people quickly showed up as first responders, a woman dressed in a party dress and two guys in white shirts/uniforms. They had to shuffle through a huge duffel bag to find the equipment they needed, seemed very disorganized. When the ambulance came, the first thing the paramedic asked me was if I was feeling a lot of anxiety lately.
I couldn’t believe it was happening to me, after reading this blog for awhile and having just read your book too! I set him straight quickly, and after awhile he realized I knew what I was talking about. It turned out I was having a case of “classic” a-fib that did show up on the EKG. Later he came into the room at the ER and told me I had done the right thing in calling. I hope he learned something from the experience.
I’m sure this isn’t your intention, Carolyn, but my biggest takeaway from reading your blog and book and also from my experience is to generally not trust ambulance people or ER doctors. I don’t understand what their training must be like if they treat any patient this way, woman OR man. Thank you for helping all of us not to be naive!
LikeLiked by 1 person
Hi Meghan – how satisfying and validating that “you did the right thing by calling 911” comment must have felt ( and I also liked the “party dress” story!) Dr. Co-Vu’s experience certainly made that particular paramedic’s behaviour sound shocking – although I’ve also heard from many blog readers over the years who have told me that it was the paramedics going to bat for them by convincing reluctant ER staff that their patients’ symptoms were likely heart-related, so dueling healthcare opinions happen…
Personally, I’ve met many paramedics since my own heart attack who are skilled and remarkably well-informed about women’s cardiac issues, so I prefer to live in hope that this one was an outlier! As for why the patient’s hubby didn’t speak to his daughter-in-law (a cardiogist), I wondered that too at first – until I figured that in many families, asking for medical advice from your own child is the default (rather than “Put Jennifer on the phone!”) Ideally every physician, cardiologist or not, would learn first thing in medical school that CRUSHING CHEST PAIN is a significant cardiac symptom!
LikeLike
This is very scary and VERY shocking. Even though there are now articles and programmes on TV about women and heart attack symptoms the message is obviously NOT getting through.
I’d better add another 5000 steps to my daily walk and reassess my diet.
LikeLiked by 1 person
I agree, Gail! The truly shocking part of this story for me (other than the realization that we should ALL have doctors in our families!) is that any paramedic would insist that a woman experiencing “crushing chest pain” is not having a heart-related problem. At Mayo Clinic, we were told that any distressing symptoms “between neck and navel that come on with exertion and go away with rest should be considered heart-related until proven otherwise…”
Not only did the paramedic apparently ignore that general rule, he argued with the woman’s son (the DOCTOR!) This was implicit bias at work, no doubt…
LikeLike
It scares me.
Had a stent for 80% blockage, symptoms SOB, extreme tiredness, fatigue, no angina as such.
Now waiting for echo after failed exercise test at 4mins, BP 228/49, new murmur, breathless, exercise stopped.
4 month waiting list for echo and holter, semi-urgent, aged 70yrs, very bad family cardiac history.
LikeLike
Hello Dianne – four months is a long time to wait for a cardiac test. Hang in there, and good luck to you…
LikeLike
Hi Carolyn,
The paramedic don’t have the right to make call here. They aren’t cardiologists and should have taken her to the hospital where she could be evaluated.
I have only gone to the hospital once by ambulance and I hated that they placed an IV line. I don’t think they would have taken me, but I didn’t have a pulse. I was diagnosed with SCD (sudden cardiac death). I now have an ICD.
I’m less then 5 minutes from the hospital and they called for a backup because I had no BP. The good thing was I was still alert and talking. I had a systolic reading of 60 with no diastolic pressure. The first diagnosis by the ER doctor was that I was over medicated .
They will never treat women fairly.
Robin
LikeLiked by 1 person
Hi Robin – it seems remarkable that you were actually able to be alert and talking with blood pressure that low, and no pulse! My understanding is that IVs are not always required in the ambulance, but some studies support a strategy that favours early pre-hospital IV in the most severely ill patients (and you certainly sounded like the “most severely ill”, wouldn’t you say?
LikeLike