 by Carolyn Thomas ♥ @HeartSisters
by Carolyn Thomas ♥ @HeartSisters
Part of what made my “widowmaker” heart attack so frightening at the time was simply how much I did not know about what was happening to me. Like many women, if I ever thought about heart disease – which was approximately NEVER! – I considered it to be a man’s problem. And as a healthy woman in my 50s (and a distance runner for 19 years), becoming a heart patient one day was never on my radar.
“What I Wish I Knew Back Then” is a new back-to-basics summer series of posts here on Heart Sisters that will revisit some of the most frequently asked questions from brand new heart patients. Today, we kick off the series with the very basic question that accompanies almost all frightening cardiac symptoms: “Am I having a heart attack?” .
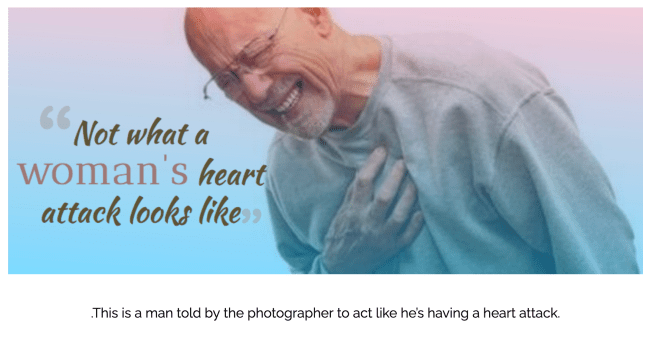
Because of my wonky heart attack stereotype (old fat guy out on the golf course clutching his chest in agony before falling down unconscious), I believed the Emergency physician who confidently pronounced,“It is NOT your heart!” before sending me home in mid-heart attack with an acid reflux misdiagnosis. But five months after surviving that heart attack, I made my first trip to Mayo Clinic in Rochester, Minnesota to attend their annual WomenHeart Science & Leadership patient advocacy training. This is what our class of 45 women with heart disease (ages 31-71) learned about women’s unique cardiac symptoms:
Warning signs that could be linked to a heart attack:
(You don’t need to have every one of these to be diagnosed with heart disease).
♥ Chest pain is the most commonly reported cardiac symptom in both men and women. But women may not use the specific words “chest pain” – even in mid-heart attack, often describing chest symptoms instead as discomfort, pressure, heaviness, burning, tightness, ache or fullness. Remember that although chest symptoms are typically a warning of upcoming heart problems, not all chest pain means a heart attack. See also: What is Causing My Chest Pain?
♥ Unusual symptoms anywhere between neck and navel that get worse with exertion, and ease up with rest: these can be felt in the chest, left or right arm (or both), upper back, shoulder, neck, throat, jaw or abdomen. Some doctors used to call these non-chest pain symptoms atypical when they happen to women. But since women make up half of the population, why would our symptoms be called “atypical”?
♥ An abrupt change in how you feel (generally described as feeling very unwell)
♥ Weakness, fainting, light-headedness, or extreme/unusual fatigue
♥ Shortness of breath, difficulty breathing
♥ Restlessness, insomnia or anxiety
♥ Bluish colour or numbness in lips, hands or feet
♥ Nausea and/or vomiting
♥ Sweating that’s out of proportion to your level of exertion or environment, or cold clammy sweats unrelated to exertion
♥ Persistent dry barking cough
♥ A sense of impending doom
Sometimes heart attack symptoms go away – and then return. When they ease up, it’s tempting to just shrug them off and go on with your day. But if they come back, seek help! These usually come on with exertion, and get better with rest – but may also start when you’re at rest.
Not all of these signs occur in every heart attack. Pay attention if these signs come on suddenly or if they feel unusual for you.
Cardiologist Dr. Sharonne Hayes, founder of the Mayo Women’s Heart Clinic, told me something surprising in an email one day: she now prefers to view cardiac symptoms in male or female patients like this:
“Focus less on symptom DIFFERENCES (which multiple studies suggest are few and can’t be relied upon for diagnosis) and more on symptom RECOGNITION by patients and by physicians, which continues to contribute to disparities in outcomes.”
During my own heart attack, I was able to talk, think, drive my car, go to work, and walk into the Emergency Department on my own steam. More on that story in this excerpt from Chapter 1 of my book.
Sometimes heart attack symptoms ease up – but then return. When they go away, it’s tempting to just shrug them off and go on with your day. But if they do come back, get them checked out!
YOU KNOW YOUR BODY!! You know if something is “just not right”.
Ask yourself what you would do if your exact symptoms were happening to your daughter or your Mum or your sister. Then do that for yourself.

What to do during unusual symptoms that could be heart-related:
- Immediately call 911 and say: “I think I’m having a heart attack!” Do not apologize for being a bother. Do not self-diagnose by saying something like: “It’s probably just a pulled muscle, indigestion, stress…” etc. Just keep saying: “I think I’m having a heart attack!”
- Chew one full-strength uncoated aspirin tablet (with water if you like) while you’re waiting for the ambulance. NOTE: Some people should not take aspirin if they’re on certain drugs, or are allergic to aspirin, or have a sensitivity to aspirin. Check with your doctor, and if you’re one of these people, skip this step.
♥
NOTE FROM CAROLYN: Please do not leave a comment asking me if I think you’re having a heart attack. I’m not a physician, so can only advise you to seek a medical opinion if you’re experiencing symptoms that feel alarming.
♥
Coming up next Sunday in What I Wish I Knew Back Then: Why cardiologists say “Time is Muscle!”
♥
ANOTHER NOTE FROM CAROLYN: I wrote much more about early cardiac symptoms in my book A Woman’s Guide to Living with Heart Disease (Johns Hopkins University Press). You can ask for this book at your local library or favourite bookshop (please support your neighbourhood independent bookseller) – or order it online (paperback, hardcover or e-book) at Amazon. And if you order it directly from Johns Hopkins University Press (use their code HTWN), you can save 30% off the list price.
See also:
-In 2021, cardiologist Dr. Martha Gulati and her team published the first ever Guidelines for Evaluation and Diagnosis of Chest Pain issued jointly by the American College of Cardiology and the American Heart Association.
–Modern medicine is male-centric medicine, and that’s a problem for women.

Hello Carolyn,
I had the pain in my neck and shoulder blades. Checking Google, I was convinced I had lung cancer. And the indigestion was just too much spicy food. Thank god I did not have a heart attack, but my widow maker artery was 89% blocked.
I was at work when I first had a symptom and I found an area to hide in till I felt better. I knew something was very wrong, but I never had a sense of doom. I had that I’m indestructible thought.
Looking forward to part two.
LikeLike
Hi Susan – Researchers tell us that women are significantly more likely than our male counterparts to engage in what they call “treatment-seeking delay behaviour” during a heart attack (like minimizing symptoms (“too much spicy food”) or denial (“I’m indestructible!”) or believing an alternative cause (“lung cancer!”)
I could really identify with your feelings of knowing something was very wrong, yet still feeling somehow indestructible. (I had two heart attacks on a 5-hour flight, knew I was very ill, yet not once did I call the flight attendants over for help. Didn’t want to be that passenger who makes the plane turn around for a medical emergency! Like you looking for an area to hide in until you felt better. Makes odd sense at the time!
Take care, hope you’re doing well now. . . ♥
LikeLike
Hello Carolyn, I have experienced the “impending sense of doom” symptom since the beginning of my cardiac issues 15 years ago.
Completely out of the blue, I will experience what I call a black depression, it can occur even in the midst of a happy day or a busy moment. One minute I am fine and the next my mood is dark and bleak.
I have figured out that when this happens I can expect chest pain, shortness of breath and extreme fatigue in the next 10 minutes. It was many years before I understood what was happening mostly due to thinking it was depression caused by my health issues until I realized that the emotion occurred so instantly that it had to have another cause.
One more “aha” moment in the process of understanding and accepting my cardiac diagnoses.
LikeLike
Hello Lauren – an interesting “chicken and egg” conundrum: does the heart condition cause the “black depression” or does the depression cause the cardiac symptoms? It’s not surprising that our physical and mental selves are deeply interconnected!
Lots of “aha” moments to be had with any cardiac diagnosis!
Take care. . . ♥
LikeLike
I must say everyone should read this. I remember one person that was an employee of the company where I’m working now, had a sudden heart attack. They were feeling something before noon, but they did not take it seriously.
LikeLike
It’s quite common – even in the middle of a heart attack – for people to dismiss or deny their symptoms!
LikeLike
Thanks Carolyn. I always learn something or get clarity on a topic when you tackle things.
When I had my heart attack, I didn’t think it was chest pain because so many of the guidelines say “central chest pain”.
My pain was up near my neck and esophagus. And it kept coming and going. Very confusing. Even “arm pain” confused me because I imagined a sharp pain on the outside of the arm and what I was experiencing was sense of pressure from armpit to elbow.
The choice of words is so important and if cardiac issues aren’t in one’s lexicon it seems so impossible. Although I have to admit I didn’t want it to be cardiac-related.
Such an education.
LikeLiked by 1 person
Hello Tomi – thanks for weighing in here on this important topic! I’m glad you mentioned getting TOO specific about heart attack symptoms.
I too have heard “central chest pain” mentioned so many times (luckily for me, I happened to have had central chest pain during my heart attack – but it still took me two weeks to force myself back to the Emergency Department after being misdiagnosed during my first visit!) And it was easier to believe that Emerg doc who sent me home because, like you, I’d rather have indigestion than heart disease! That central chest pain also seemed to reach up into my throat and neck – which reminded me of the kind of pain I used to experience during long runs up steep hills, which I just chalked up as a “normal” lung – not heart – response.
Best not to split hairs (e.g. Q: is it central chest pain, or left chest pain, or right chest pain we should pay attention to? A: it’s ANY pain or discomfort between neck and navel!) And as you say, this pain or discomfort may or may not come and go – it IS confusing!
As I quoted Dr. Hayes: symptom RECOGNITION by both patients and physicians is smarter than trying to keep track of symptom DIFFERENCES!
Take care, Tomi. . . ♥
LikeLike
Thank you for sharing these descriptions!
What is feeling “an impending sense of doom” in this context? I’ve seen that description before and can’t quite get my arms around the meaning as it relates to a cardiac event.
LikeLiked by 1 person
Hello Marsi – this does sound like an odd symptom, doesn’t it? But many women have described this sign during their heart attacks, often accompanying constricting pressure in the chest – an extremely strong feeling that “something is very wrong with me” – and that something bad is happening or will happen soon. For many women, it’s the one symptom which ultimately convinces them to seek help. Most women I’ve met are very skilled at minimizing their symptoms and talking themselves out of seeking medical help!
It’s why I suggest that any women in this situation first ask themselves what they’d do if their daughter or their Mum or their sister were reporting that same strong “something is very wrong” sense of doom. Most likely, we’d want them to trust that gut feeling.
Take care. . . ♥
LikeLike