 by Carolyn Thomas ♥ @HeartSisters
by Carolyn Thomas ♥ @HeartSisters
I’m wondering how many more cardiac studies published in medical journals we’ll need before medical professionals start believing what decades of published research have already concluded. Here’s just one example: British researchers have described those past conclusions as: “an undeniable gender-based inequality in cardiovascular health to the detriment of women.”(1)
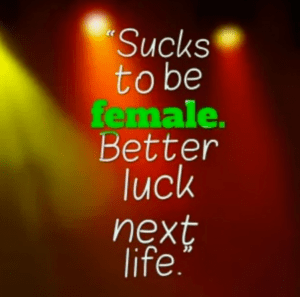
At this point, I can’t help myself. Whenever I come across yet another heart study that comes to that identical conclusion, I have to quote my irreverent and brilliant heart sister Laura Haywood Cory, who at age 40 survived a heart attack caused by Spontaneous Coronary Artery Dissection (SCAD). No matter the specific focus, Laura interprets those “ain’t it awful?” cardiac research conclusions like this: “Sucks to be female – better luck next life!”
And a feisty challenge comes from McGill University professor Dr. Cindy Blackstock to her academic colleagues as she expressed in a University Affairs interview.
“Don’t just publish another paper. Let’s DO something!”
Dr. Blackstock is echoing the message of a paper published in the Journal of the American Medical Association (JAMA) that explored why a relatively new research field called implementation science seeks to narrow the cavernous gap between published research on medical practices and the eventual accepted integration of those practices out in the real world with patients like me(2):
“Historically, this research-to-practice gap, and whether these findings actually translate into public health impact has not been the concern of academic clinical researchers.”
Whaaaat? Not the concern of academic clinical researchers?!?
NOT THEIR CONCERN?!?
That study on implementation science published in JAMA reminded me that I’m not the only one wondering how academics who don’t care if their research makes a difference are attracting funding in the first place – although it seems that some people do care a lot. For example:
“Funders of biomedical research have been concerned over the lack of public health impact of their research dollars.”(2).
In 2010, I started writing about this gender-based inequality in cardiology. My first article was called: Heart disease: not just a man’s disease anymore.
My second was written the same year. Still gender disparities in treating women’s heart attacks
And so was my third: “How doctors discovered that women have heart attacks, too“
And they just keep on coming, year after year – as more remarkably similar research studies on these gender disparities keep getting published. The question I ask every time is “WHY IS THIS STILL HAPPENING?”
I often feel like I’m reading the same medical journal article – over and over. Different lead authors, different sleep-deprived grad students, different universities, different publication dates, different cardiology journals – but essentially the same “ain’t it awful?” study.
I’d like to highlight some of the U.K. researchers’ specific observations, particularly their suggestions for addressing this gender-based inequality that I’ve been writing and speaking and obsessing about since surviving my own misdiagnosed heart attack back in 2008. I’m not a physician or an academic, but these are simply some issues I’ve been pondering for a long time:
♥ U.K. research highlight: “With such damning evidence that women are under-represented and indeed under-treated, the time has come now to question whether women should be considered as their own specialty within cardiology.”
(What I’d say: YES, THE TIME HAS COME! What are we waiting for? When can we finally stop asking the same question that’s been asked for years? See also: Does Your Hospital Have a Women’s Heart Clinic? If Not, Why Not?)
♥ U.K. research highlight: “In order to reverse this disparity, it is clear that further research is required to improve treatment of women.”
(What I’d say: HOW MANY MORE PUBLISHED STUDIES DO WE ACTUALLY REQUIRE? Why aren’t we acting on the conclusions of countless previous studies suggesting the same thing? See also: Implementation Science: Should Research Actually DO SOMETHING? 2023)
♥ U.K. research highlight: “We need to enable the development of sex-specific strategies and clinical guidance to empower clinicians moving forward.”
(What I’d say: CARDIAC PRACTICE GUIDELINES ARE ALREADY IN PLACE! Clinicians are not only “empowered” to follow current guidelines, non-government organizations like Accreditation Canada (where I live) should ensure that appropriate adherence to existing guidelines for both male and female patients is part of their annual hospital accreditation process. And as Dr. Sian Harding, a respected British cardiac researcher for over four decades, wrote in her blistering 2022 essay in The Guardian:
“Once a heart attack is suspected in a patient, the standards and guidelines for treatment are well defined. Doctors should be recognizing heart disease in women and giving them the optimum standard of care. However, this is not happening.”
♥
♥ U.K. research highlight: “It is time for healthcare professionals to recognize that the old ‘one-size-fits-all ‘cardiac approach is no longer acceptable, especially when delays in cardiac diagnosis and treatment are a common occurrence for women.”
(What I’d say: “DOES ANY DOCTOR TRULY BELIEVE THAT WOMEN ARE JUST SMALL MEN? If current doctors accept that, it suggests that med school has failed them. Maybe future researchers might swivel their focus to study doctors who cling to that belief, and to medical schools who will correct that belief before it takes root. See also: Nine lessons about women’s heart disease that future doctors will learn in medical school).
♥ U.K. research highlight: “With emerging conditions such as spontaneous coronary artery dissection (SCAD) predominantly found in women, a better understanding is needed.”
(What I’d say: SCAD IS NOT AN “EMERGING CONDITION.” SCAD was first described in 1931 at a postmortem examination of a 42-year-old woman. And as cardiologist, SCAD researcher and founder of the Mayo Women’s Heart Clinic Dr. Sharonne Hayes has observed: “We once believe that SCAD is rare. We now believe that it’s rarely correctly diagnosed.” ) See also: How I Used to Describe SCAD. And What I’ve Learned Since.
♥
In spite of this U.K. study – and countless other published studies – we continue society-wide to tolerate a medical system that is pervasively male-centric.
We tolerate diagnostic tests, cardiac procedures, powerful drugs and implantable devices that have been developed, studied and approved for (white middle-aged) men. See more about what female patients have had to tolerate in Dr. Alyson McGregor’s important work: Modern Medicine is Male-Centric Medicine, and That’s a Problem for Women.
And if you happen to be one of those sleep-deprived university grad students who is deciding your thesis topic, here’s my cautionary plea:
Instead of spending years on yet another “Sucks To Be Female” PhD thesis or future journal submissions, why not revisit your research focus? Grad students often say that choosing a thesis topic is the most challenging part of work that will take up the next three years of your life. You could make the decision to study cardiac issues that can actually help move the needle – like why cardiac diagnostic tests that work pretty well in men aren’t as accurate in women – who are being sent home because their test results seem “normal”. Become part of a research team that wants to accomplish more than rehashing prior journal citations. In other words, DO SOMETHING!
Here’s a concrete example of how that can look in real life: Vancouver cardiac researcher Dr. Karin Humphries and her team have been studying overlooked issues with the commonly used high-sensitivity blood test for a cardiac enzyme called troponin.(3) Troponin is rarely detectable in blood tests -but if your heart muscle is damaged by a heart attack (or possibly if you’re an endurance athlete who enjoys competing in Iron Man triathlons!) troponins can leak into your bloodstream and your troponin blood levels will rise. A rise in troponin levels has typically been a standard marker for heart muscle damage during a cardiac event.
But the troponin threshold commonly used in this test is based on a level that’s considered appropriate for men, but may be set too high for women – meaning that even our positive blood tests can be misinterpreted as “normal”. Dr. Humphries has found that “setting a lower female-specific troponin threshold would improve the diagnosis, treatment and outcomes of women presenting to the Emergency Department.”
.
-
Bosomworth J, Khan Z. “Analysis of Gender-Based Inequality in Cardiovascular Health.” Cureus. 2023 Aug 14;15(8):e43482.
-
Rubin R. “It Takes an Average of 17 Years for Evidence to Change Practice—the Burgeoning Field of Implementation Science Seeks to Speed Things Up.” JAMA. 2023;329(16):1333–1336.
-
Zhao Y, Humphries KH et al. “High-Sensitivity Cardiac Troponin – Optimizing the Diagnosis of Acute Myocardial Infarction/Injury in Women (CODE-MI): Rationale and design for a multicenter, stepped-wedge, cluster-randomized trial.” Am Heart J. 2020 November. 229:18-28.
♥
Q: Is there a heart-related topic that you’d like to see more focused research on?
woman + man image: Quinn Brak, Pixabay
NOTE FROM CAROLYN: I wrote much more about implicit bias in cardiology in my book, A Woman’s Guide to Living with Heart Disease. You can ask for it at your local library or favourite bookshop (please support your favourite independent booksellers) or order it online (paperback, hardcover or e-book) at Amazon, or order it directly from my publisher, Johns Hopkins University Press (use their code HTWN to save 30% off the list price).

And to continue my rant, some EMT personnel make a “diagnosis” simply on EKG or impression, and bias the ER staff before you arrive. I know I’ve mentioned being forced to climb out of ambulance and walk into ER mid heart attack.
LikeLike
Helen, I remember when you shared that dreadful experience here – I often repeat your story that, sadly, is not unique to you.
A number of readers have told me of paramedics who didn’t exactly refuse to transport them to the hospital during their heart attack, but kept making comments to them like: “Are you SURE you really want to go to Emergency?” until the patient – now embarrassed because “Even this paramedic thinks I’m making a fuss over nothing! ” – said, “Well, maybe not. . .”
But YOUR story takes the cake!
Take care. . . ❤️
LikeLiked by 1 person
I guess I’d like to see more research on cardiac microvascular disease and definitive diagnosis and treatment.
At least it’s no longer called Cardiac Syndrome X. But in my experience, because it does not “show up” on a regular cardiac cath, it can’t be proven and is a possible diagnosis left unmentioned.
My cardiologist never mentioned it as a possibility until I asked directly “Could these chest pains be caused by microvascular disease?”
LikeLike
Hello Jill – You were smart to ask that direct question out loud!
In the wonderful world of cardiology, coronary microvascular disease is still a new-ish diagnosis (first identified by researchers who described 10 patients with angina but normal or near-normal angiograms – and labelled them as “group X”). In 1973, describing this patient group, the late Dr. Harvey Kemp in New York City first used the name Syndrome X to describe the uncertain cause of that chest pain.
One of my readers told me that when she asked her own doctor the same question (could my symptoms be due to coronary microvascular disease?) – he responded: “I don’t believe in coronary microvascular disease!”
So you were also lucky that your doctor was a believer.
Take care. . . ❤️
LikeLike
My cardiologist is a specialist in women’s cardiology. I saw her recently and told her about being out of town on vacation a few weeks earlier and awakening with severe indigestion, pain, and a few hours later angina.
I STUPIDLY didn’t go to the ER. Why? Because I have a “rich” cardiac history and have spent too much time in ER’s only to be dismissed and sent home or misdiagnosed and then identified correctly down the road.
I just couldn’t face sitting in a hard chair in the ER feeling awful. Not a new story. So, after scolding me (appropriately) for not going to the ER she had a GREAT suggestion: she told me to print out her visit notes, keep it in my purse and give it to the ER if/when this happens again, AND to insist on 2 high sensitivity troponin tests.
Those who haven’t yet had a heart attack could print out a list of women’s heart attack symptoms, keep in their purse, hand it to ER staff and insist on troponin tests.
And yes, I may have had another heart attack- will know more after upcoming echo.
LikeLike
Hello Helen – yoiks! Sorry to hear about that scary episode – not scary enough to send you to Emergency, though! I can understand completely your reluctance, of course: it’s awful to keep going back to Emergency after being dismissed so many times before.
I met a woman when I was at Mayo who, like me, had been misdiagnosed in mid-heart attack and sent home from Emerg. But UNLIKE ME, she was much smarter – and kept going back, repeatedly saying: “I know my body, and SOMETHING is very wrong with me!” On her 3rd trip back, she was offered a prescription for anxiety meds. On the 4th trip, she underwent triple bypass surgery.
Your doctor’s suggestion to keep your appointment notes to give to Emergency staff in the future was a good one, but even insisting on those 2 troponin tests may not help UNLESS your Emerg docs are familiar with Dr. Karin Humphries’ studies that have found that even the high sensitivity troponin test thresholds are set too high for women.
“Dr. Humphries has found that “setting a lower female-specific troponin threshold would improve the diagnosis, treatment and outcomes of women presenting to the Emergency Department.”
Maybe instead of sharing your cardiologist’s appointment notes next time, you could print off and share a copy of the Humphries journal publication.
Good luck at your echo appointment!❤️
LikeLike
Probably printing both her notes AND the journal article – as to look at me, no one would guess I have Fibromuscular dysplasia (FMD), cardiac puncture, 2 cardiac arrests, 2 renal artery dissections, 2 kidney infarcts, possible coronary artery dissection, one maybe 2 heart attacks now – they look and see a slightly overweight elderly woman appearing in decent shape – and assume it’s me being “nervous”.
LikeLike
Oh yes! Many doctors seem to have magical powers that allow them to diagnose from afar – simply by looking at us. The Emerg doc who misdiagnosed my heart attack told me: “YOU are in the right demographic for acid reflux!” before sending me home. ❤️
LikeLiked by 1 person
To Helen:
I too have the look of a slightly overweight elderly woman whho appears in decent shape. As a doctor comes in to visit me, behind that awful curtain in the ER, I can almost FEEL him thinking “Well, she looks in pretty good shape to me – let’s see how fast we can get her out of here and get a REAL emergency into this bed.”
I know this isn’t true for every doctor in the ER, but it’s happened enough times to me that I do avoid the ER as much as possible. Which is not good for those of us with tenuous health issues. Sending you good wishes and hope for good doctors!
LikeLike
Hi Jill – I wonder if Emergency Department staff even know what it sometimes takes to propel most patients into their hospital to seek urgent care – even when they really need help!
In my experience, going to Emerg (e.g. waiting endlessly, surrounded by crowds of sick, crying, bleeding or injured people, and risking the very predictable likelihood that your symptoms will be dismissed or denied or misinterpreted after all that) is mostly the last thing any of us want to do before forcing ourselves to go in – even when, as you say, it is NOT GOOD decision-making for “tenuous health issues”. ❤️
LikeLike