by Carolyn Thomas ♥ @HeartSisters
Summer Ash is a self-professed space cadet. She’s an astrophysicist at Columbia University’s Department of Astronomy in New York City, where she serves as the Director of Outreach.* Five years ago, she underwent open heart surgery after she was diagnosed with an aortic aneurysm (that’s when the tissue of the aorta balloons out dangerously). This condition was likely linked to a congenital heart defect Summer was born with called a bicuspid aortic valve. About 99% of people, as she explains, are born with a normal tricuspid aortic valve (meaning three leaflets in the valve), but she was one of the 1% born with only two. With her kind permission, I’m running her story here as it was originally published on her blog, Defective Heart Girl Problems.
♥
“I think there is a big misconception about how fast ‘young people’ heal from a surgery like this. There’s healing and then there’s HEALING. On one hand, being young and strong and in good health (with one obvious exception) means I can physically heal faster than the average open heart surgery patient.
“On the other hand, the average open heart surgery patient is much older and often in poorer health – so much so that doctors often find a less invasive way to operate on the heart: a partial-sternotomy, a thoracotomy in between the ribs, or even going in through the femoral artery, all of which are less invasive than a full sternotomy.
“My surgeon said that since I was in such good shape, he would just go the direct route. My body could clearly take it. I would ‘bounce back’.
“Lucky me.

“Turns out growing new bone between my sternum wires, reconnecting my muscles and nerves across my chest, and regaining my strength was the easy part. It’s at least straightforward. There’s a checklist of things to do: sit up, stand up, walk, walk again, and walk some more. Keep walking. It may not be linear (it most definitely was not), but at least there’s a path laid out for you. Millions of people have healed from this before. Six weeks after leaving the hospital, my surgeon declared me fixed and told me to go live my life.
“But almost two years later, I’m struggling to do just that.
“My surgery was on the books and over with well before my mind even accepted it was happening. I focused all my energy on understanding what would happen to me physically and I didn’t stop to consider what might happen to me emotionally.
“Sure I had the occasional breakdown while recovering, but it almost always stemmed from pain and fatigue and frustration. It wasn’t until six months later that the first cracks began to show while I was organizing my medical bills in preparation for filing my taxes. I had a massive envelope full of receipts and I was entering them into a spreadsheet, all out of order.
“The second after I typed the entry “taxi to hospital” for the morning of my surgery, I completely broke down. It was as if all the fear since I found out about my aneurysm had been filed away in a corner somewhere and I had just stumbled upon it. This happened a few more times and then it ended as suddenly as it began and I thought nothing more of it.
“A year later, it all resurfaced, only this time it came in waves, each one bigger than the one before. I started to have visceral reactions to things that reminded me of surgery, both directly and indirectly. I felt other people’s pain as if it were my own.
“When once I had no trouble watching medical dramas, I now actively turned away from scenes in the OR. I had to skip over the news items in my Facebook feed from the two heart surgery groups I was a member of. I started avoiding my godparents’ neighborhood on the Upper East Side where I stayed during my recovery. Every time I crossed Park Avenue, I would have a flashback to when I couldn’t make it across the intersection in one cycle of the light. Riding in a taxi only made me remember how vulnerable I felt being in a car after surgery. If I saw anyone in the subway walking with a cane, I would immediately remember how terrified I was of being jostled when I started commuting on my own again. I started feeling the need to adopt a defensive posture and protect my chest again.”
“The city became a minefield. My mind became a minefield. It was so bad at one point, even seeing the shape of a heart (anatomical or symbolic) would trigger me.
“And my bionic heartbeat morphed into the worst trigger of all: one that I couldn’t escape. It went wherever I went. It was inside of me.
“Something had to be done.
“There is nothing medically wrong with my heart so no procedure or prescription could do anything about the pounding in my chest. As an alternative, my GP suggested clinical hypnosis or biofeedback as a way to try to transform it into more of a background sensation. I had heard of biofeedback before and it piqued my scientific interest so I decided to explore that option first. That’s how I found Dr. Leah Lagos, a psychologist trained in biofeedback, who I’ve been working with since mid-March.
“Through working with Dr. Lagos, I’ve come to realize two things:
- All the of emotional and visceral reactions I mentioned above are actually symptoms of post-traumatic stress disorder (PTSD). I approached my surgery as a logical, medical necessity and focused all my energy on planning the practical steps for my recovery. I spared little or no energy for what I thought about needing to have my most vital organ repaired. My rational brain took the wheel and relegated my emotional brain to the back seat. As a result, my body, and my heart, actually experienced my surgery as trauma. Which makes a lot of sense when you think about what my body actually went through: my torso was sliced open, my sternum sawed in half, my ribs forcibly spread apart, and my heart was stopped. Yes, all these things saved my life. My rational brain knows that and accepts it. But ever since I woke up in the ICU in tremendous pain, my emotional brain (via my heart and my body) has been screaming “WTF?!” – which ties into #2…
- I’m fucking pissed at my heart for letting this happen to me.
“At first I thought my bionic heartbeat bothered me so much because it felt like something must still be wrong. Why else would it be so loud and so forceful? Surely it must be trying to tell me something. But it’s not fear it triggers, it’s anger. Really raw anger.
“When something starts going wrong in your body, you usually get some kind of clue: a twinge, a pain, a change. Something that hints at a difference. Something that tells you things aren’t quite right. Something that makes you think twice. Nothing like that occurred here. Nothing at all. My aorta was expanding and stretching to its limits and my body never said a word.
“My heart, the organ that gives me life on a moment to moment basis, lied to me. It violated my trust. When it was in grave danger it sat in silence. Now it’s perfectly healthy and it won’t shut up. I don’t know what to believe anymore. I’ve lost all physical confidence in my body.
“So that’s where things stand at the moment. The biofeedback is helping me make great strides on both these fronts, but it’s an ongoing process.”
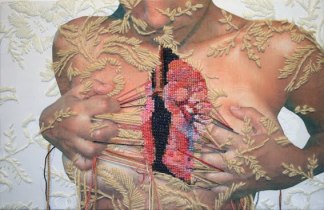
Image credit: Ana Teresa Barboza
Q: Have you, like Summer, had the experience of “sending your emotional brain to the back seat” during a medical crisis?
♥
NOTE FROM CAROLYN: I wrote much more about the link between heart disease and mental health issues in Chapter 5 of my book, “A Woman’s Guide to Living with Heart Disease” . You can ask for it at your local bookshop, or order it online (paperback, hardcover or e-book) at Amazon. Or if you order it directly from my publisher, Johns Hopkins University Press (code: HTWN), you will save 30% off the list price when you order).
♥
* Since this post was published, Summer is no longer a New Yorker. She has moved to a new home and a new job! She’s now the Senior STEAM Education Specialist for the National Radio Astronomy Observatory in Socorro, New Mexico.
See also:
The day I made peace with an errant organ
Six personality coping patterns that influence how you handle heart disease
How we adapt after a heart attack depends on what we believe the diagnosis means
Not just for soldiers anymore: PTSD and heart disease

I had open heart surgery on March 5, 2019. I went into it with a pretty cavalier attitude. When I woke from surgery, in the throws of horrible hallucinations, my first thought was, “This is not at all what I expected!”
Of course, I had no expectations because I had no frame of reference. The hallucinations lasted 3 days and during that time my blood pressure bottomed out and I lost the ability to breathe.
Everyone kept telling me how wonderful I was doing so I knew they had no idea the pain I was in. By the fourth day, I was in less pain. And then I went home on day seven. Everything I did hurt and when I had trouble breathing, I was scared to death I would stop breathing again.
I started cardiac rehab this week and I was pretty sure I would do something wrong and die. But, oh my goodness, I didn’t die and I felt better afterward. I still have quite a journey ahead that will require me to work harder than I ever have.
I see the light at the end of the tunnel now and it hints of many more years of life with my children and grandchildren. I try to keep the fear away with a positive attitude and each day is a little better.
LikeLiked by 1 person
Thanks for sharing your unique perspective here, Suzan. You’re in very early days yet, but seems like you’re already feeling far less of that fear and pain. No wonder you had a ‘cavalier’ attitude going into this experience – until you’ve actually had the experience, there’s no way to appreciate the reality, and those hallucinations sound scary!
I’m so glad that you’re in cardiac rehab now – this is a remarkable program that researchers have found produces significant improvements in longterm outcomes. Best of luck to you!
LikeLike
Thanks for the wonderful article.
LikeLike
Summer, I can’t thank you enough for this amazing article. Unaware I was born with BAV I developed a cardiac infection. Open heart surgery, two valves replaced and a Pacemaker.
Physically yes, healed very well. It’s now been two years physically good. Emotionally scarred from it all. The nightmares are always final, fronting Death.. It’s like my brain is trying to recall what happened.
Thank you again
Catherine Baker 😊
LikeLiked by 1 person
I loved this article.
Had my third open heart surgery. It will be Feb 1 2019 in 17 min. I am again wide awake. My anxiety is so bad my jaw is going out of place. My pharmacy changed my generic Restoril brand for sleep in Dec. My primary care wrote me a script for brand only. I think that after a 15 hour surgery I am going to die from insomnia and anxiety. The pharmacy will not fill the brand Restoril, they said it’s not up to my doctor or up to my insurance it’s up to them.
I bought a bite guard today so I don’t break my teeth and my jaw can stay in alignment so I can eat my granola in the morning. After each open heart surgery my anxiety and insomnia get worse. I am out of rehab for a bit because in Jan I had to go back in for an ablation.
I am a registered nurse. Before my first surgery I was telling doctors something was wrong. After 6 years of trying, they found the hole in my heart. This past July I was telling doctors my breathing had changed. One doctor told me I don’t breathe deep enough, another one told me to elevate the head of my bed.
From July to October I became critically ill. I ended up being sent for a TEE and the nicest female cardiologist would not let me go home. I had a 15 hour surgery A repair of an ASD. Replaced Mitral Valve. The ring of the old one was gone. An aortic valve replacement and a Tricuspid Valve repair and a pacemaker put in.
I try to explain my feelings to some and everybody just tells me how good I look. That’s not what I want to hear.
I don’t feel good yet. If I live long enough I will need a new pacemaker and new valves. I don’t think I can endure another surgery. I am sorry for going on for so long, I thought this article really hit home for me. Thank you for writing this.
LikeLiked by 1 person
Hello Joanne and thanks for sharing your unique and overwhelming story. You have officially surpassed your maximum lifetime quota for traumatic things happening to your body! And it’s often the “one more thing” burden that seems impossible to bear after enduring this many events and procedures – even though each procedure is necessary to help you.
Even issues like needing a bite guard can simply feel too much to take. I can’t even fathom what your pharmacist is saying: it’s not up to the DOCTOR to decide on the prescribed meds? I thought that’s exactly who decides!
I hope you will consider professional talk therapy Joanne, somebody to help you through this suffering. You have far more than physical pain you’re dealing with. Best of luck to you…
LikeLike
Hi Summer,
I was looking around the internet to see if I could find another heart sister who has experienced some of what I feel I am going through. Like you, I am a vibrant young(ish) woman, who has recently been through open heart surgery, and trying to find that confidence in my body again.
I was recently handed the book, “The body keeps the score”, to help with some of PTS, but would love to actually talk with someone who has been through a similar experience. I certainly can relate to your story.
I’ve been trying to heal emotionally so I can now look ahead with confidence and have my shoulders relax. I’m just not there yet… but really want to be. Any suggestions would be most welcome.
LikeLike
I’m preparing for possible open heart surgery and I’m normally able to think and research my way through the medical facts and come to a decision that I could live with (no pun intended). At 76 years of age I’ve always tried to make my medical decisions on my own. But people close to me won’t back the f… off and this is making me lose sleep and raises my anxiety even more.
Having gone through coronary angiograms and having worked in the medical field for over 20 plus (CT and x-Ray) years, you would think people would let me figure out and give me some space. But I have people from all over calling and urging me to do what they think is right, which only makes me more angry, because they don’t understand how personal this is. How do I resolve this? I know they mean well but they’re really starting to piss me of.
LikeLiked by 1 person
Hello izapx – I hear ya! I too am shocked by how people (some who don’t even know you!) feel quite free to offer unwanted opinions on how to live life as if it were somehow their business what we decide. You’re right, often such unsolicited advice stems from a need to be helpful, but honestly, do they think we haven’t already weighed every option, every decision, every scenario ten times over?
LikeLike
My thoughts and prayers are with you, izapx. My story is one that haunts me to this day, and I am 13 months post surgery.
I had thyroid cancer 15 years ago and my thyroid was removed. For years I was tooling along at the same Type A plus level that I had always lived. In July, just one month after I had one of my bi-annual doctor visits I began experiencing symptoms. At first it was dizziness with occasional nausea — almost every day. Within a couple of weeks the fatigue set in. It was so pervasive that I would spend my lunch hours in my car laying back trying to rest. A month or so later came the feeling that I was walking through sludge. And the final symptom was the overwhelming heaviness in my limbs.
I went back to my Endo doc almost immediately; he told me it wasn’t my thyroid. The early symptoms mirrored my thyroid issues so much that I was convinced he was wrong. I went to Web MD (little help) and found that it could be one of about 500 things. I returned to my Endo doc and he repeated that “my blood work was perfect” and IT WAS NOT my thyroid.
I felt like shit almost every day and I had no idea where to turn, so I began keeping a diary of the daily symptoms and events. I will mention that while this was going on, I was also experiencing stomach issues. Sometimes so badly that the cramping and pain led me to believe I might have pancreatic cancer or pancreatitis.
I FINALLY found an internist who dismissed that theory and was working to solve the puzzle, and then I had an incident at work where 911 was called. The pain in my stomach was so bad that I literally thought I was dying. I was taken to the ER and it was there that they casually mentioned I might look into visiting a cardiologist because I had nearly crashed. Two days later a co worker diagnosed me and I took myself back to the ER (lying) and saying I was having a heart attack. In essence I spent five months searching for answers, and not a single doctor noticed there were problems with my heart.
Until this blog, I didn’t realize that only 1% of people are born with a bi-cuspid valve, and also like Summer’s story, I am a practical person that thought I would breeze through this with only minor issues. WRONG! I continue to feel crappy. My cardiologist thinks I need to take anti-depressants because they are convinced that is why I still feel dizzy and nauseous. I will tell you that I stopped taking the metoprolol and atorvastatin pills because those made me sicker, but I STILL don’t feel 100% and I feel like I’m going crazy.
I’m sorry for blathering all of this, but I guess the point is that I never stopped trying to find the answer and it took ME and a co worker to figure out what doctors and friends could not. I am strongly leaning toward the therapist route because I do get depressed and frustrated.
I hope you figure out what works best for you, and that you will know exactly what to do.
LikeLiked by 1 person
Very key message, Jeannette – “never stop trying to find the answer!” Again, best of luck in finding that therapist – one of the best things I ever did…
LikeLike
Great story from another survivor of open heart surgery. Hope you can keep on with your career and overcome the fears.
LikeLike
With absolutely no warning I ended up having open heart surgery in March 2018. People are impressed with my speedy recovery. they don’t see what is going on in my psyche. I am angry and afraid and sad. every day. nearly every hour. no resource previously helpful has altered my emotional state at all. I feel all alone. I want help but have no idea where to go for it.
LikeLiked by 2 people
Hello Linda – I’m sorry you are going through all of this. You can guess by reading Summer’s story and many many other blog posts here that you are not alone – and it’s somehow made even more troubling by looking so “normal”. I used to wish sometimes that I could wear a neck brace or a leg cast!!
And you are in relatively early days yet – just over two months. It’s very common to feel utterly overwhelmed at this time while you’re trying to make sense out of something that just makes no sense at all. You WILL start feeling better over time (you may not believe that now, but you WILL!) Most mental health issues brought on by a cardiac event are what’s called “situational” – almost always temporary and treatable.
Make an immediate appointment with your physician for a referral to a professional therapist/counselor/cardiac social worker and tell him/her exactly what you’ve been going through. Many physicians are simply unaware of this very common post-discharge experience! Meanwhile, read this excellent <a href="https://myheartsisters.org/2010/05/18/surviving-crisis-heart-attack/”>4-part excerpt from Dr. Wayne Sotile’s book “Thriving With Heart Disease”.
You can also find lots of online support (over 37,000 women with heart disease, all over the world) at the WomenHeart online support group – it’s free to join, and open 24/7 if you want to post a question or a comment Best of luck to you…
LikeLike
Not sure but sometimes sitting back and getting a grip on yourself and knowing that you’re basically, except for the problem at hand, in fairly good health, as most of us are these days, might help you believe that this is just another hurdle in life that you’ll have to face and realize its not insurmountable. Know that the people in your life really care and its probably tearing them apart also. You may feel that you’re facing it alone but someone close to you may not be saying anything but if you look closely you’ll see that you’re not by yourself. Reach out if need be and you might be surprised. Good luck and God Bless.
LikeLike
Hi! I’m 8 years out from open heart surgery to repair a mitral valve, it took time and plenty of therapy to get over it. I hope you are doing well, I had very similar issues, if I saw anything that reminded me of my surgery such as a pair of nonslip hospital socks, purelle hand sanitizer, or even movies I watched in my recovery room I’d get cold sweats which often turned into full blown panic attacks.
I just want to let you know that with time and therapy it’s possible to be fully cured of this trauma. I now can go in hospitals or to my cardiologist as if they never did anything terrible to me there.
LikeLiked by 1 person
Hurray! You did it! I only wish medical professionals were able to offer patients acknowledgement and support for this response long before it gets that severe…
LikeLike
I would like to share my story just to see if how I’m feeling is normal
I’m 63 years old and had a triple heart bypass 4 mths ago after having two heart attacks out of the blue, never had heart problems. Even after 4 mths I’m still tired all the time and my chest and scar are still painful.
I’m so traumatised with what happened to me in hospital. I had a collapsed lung and pneumonia during the operation which meant I had these awful masks I had to wear for 10 days to help me breathe. I’m so fed up with still feeling tired and depressed and I feel like my life will never get back to normal. I’ve gone from being an active rushing about kind of person to not wanting to go out because it takes so much effort. Is there anyone else who is taking a long time to heal and get back to normal??
Lorraine xx
LikeLiked by 1 person
Hi Lorraine – I’m sorry you are not yet feeling back to your old self. You might be surprised to know that your experience is actually not uncommon. Your body is recuperating not only from two heart attacks, but open heart surgery and – as if all that’s not traumatic enough – a collapsed lung and pneumonia, too! No wonder you are feeling so tired and depressed.
Every patient is different, and there is no specific guaranteed timeline for speedy healing. Many patients recovering from cardiac surgery say that it can take 6-12 months to start feeling ‘normal’ once again. You are in very early days yet at just four months post-op (especially given your other complications). Fatigue can take a while to pass. Take one day at a time, try to get outside for fresh air (even a slow short walk). Yes, you’re right – it is an effort to get up and out the door, but every bit of exercise you do each day now will help you feel better day by day. In other words, the less you do, the worse you’ll feel and the less you’ll want to do. If your chest pain continues or gets worse, mention it to your doctor. Meanwhile, you might be interested in visiting the WomenHeart online support group. It’s free to join and you can ask lots of questions and learn from many many other women who share your experience, too. Best of luck to you…
LikeLike
As I read Summer’s story, within a paragraph or two my brain said ‘PTSD’! How could she not have it with all that happened? And doing a major operation, when the surgeons could have been cautious and careful, seems to me the height of, if not malpractice, then total disregard for the patient.
My husband had a quadruple bypass in 1998, and has since had three stents, so he was the ‘cardiac patient.’ He’s NEVER had a side effect from a medication (that he would admit). Instead, he sets up experiments with the cardiologist after he reads papers, the cardiologist lets him try different drugs or combinations, and then they evaluate the results together!
Nobody told me depression is a common occurrence after the three stents I just got – in a very badly-managed two-week ordeal. I’m certainly not in Summer’s class – but I’m also much older and have had CFS since 1989, and the whole ER experience was highly traumatic, and complicated by reactions to every drug (I warned them – they didn’t listen).
It’s just too much to handle. I don’t tolerate antidepressants, and don’t have the energy to ‘go talk to someone,’ so I’m handling it with CBT (good at that after all these years). I hope the cardiac rehab I’ve agreed to (and will control with an iron fist so as not to exceed my CFS guidelines) plus the better blood flow will actually end up with me in a better place. I dumped the first place after talking to the guy in charge (drill sargeant) on the phone. The biggest hospital, etc., problem? CONSTANT new people ordering me around, thrusting drugs at me, and expecting me to fall in with their plans (different for each nurse). And then telling me I had to make the choice – and having me sign ‘informed consent’ forms. What a lie.
I’ll get there – grateful to be alive – as soon as I can. I hope to find more stories on this blog to help me process.
LikeLike
Alicia, it can for sure feel like “too much to handle”. I’m glad to know that you’ve been referred to cardiac rehab, which has been shown in study after study to reduce mortality rates by up to 30% (that’s right up there with statins!) If you can go into that program with a willingness to trust the process, you too will find significant benefit. If you go in with your dukes up ready to interpret instructions as “ordering you around” – well, then you can’t expect much success, frankly. They’re not ordering you around, they are helping heart patients who are afraid to move start moving a little bit. We know that sustained anger and hostility (especially directed at the people who are the ones trying to help) can ultimately negatively affect outcomes for heart patients. Try to lighten up when you walk into your first few rehab classes. Protect your own physical capabilities, of course, but please be willing to be curious, not furious…
LikeLike
As you say, you know your disease far better than most people you will run into in the medical profession, even in cardiology. It matter to you. I don’t know what your limitations are as far as rehab and exercise, but you do – and they may not. Not well enough not to harm you. I think you are your own best advocate – and even you are pushing boulders up hill.
I have 27 years of doctors not handling the CFS properly. I spent time on the phone with the people in charge of both rehab programs I am considering. Neither place had anyone with any knowledge, or prior patient they could refer me to for a reference.
The second was more maleable, by far, than the first, so that’s where I’m going. It may be just as bad in practice – I could not get a straight answer to the question, “Will I be able to SEE my heart rate as I’m exercising?” until I had asked it eight times, and finally got the answer, “No.” And they don’t maintain their bicycles, so that is not reliable – on the only machines they have with a HR display.
When I tell them that I will crash if they try to raise my heart rate into the aerobic region, because my body can’t produce energy aerobically, they don’t get it. I can’t educate every single PT person in the programs, but I can insist on knowing my HR (I’m taking my chest strap monitor, and their electrodes will have to work around that), and making sure I don’t go over my limit (93-95 BPM).
Then I can work for longer periods each time, starting at a few minutes with huge rests in between. I have the papers for them that explain how and why. They wouldn’t let me send them ahead.
I have huge dread – and will have to just do my rehab at home if they can’t work with me. But don’t blame the patient when the PT people won’t listen. We’re cleaning the basement (my assistant is, not me personally) so there is room to use the machines we have down there, and I can use the Nordic track sitting, and the rowing bits and weights on the other machines.
I’d rather do it at the rehab place – in the same building with the ER – but I’ll do it my way rather than not at all if I can’t make them listen.
I know I sound nuts – and I apologize for monopolizing your blog comments – but I’ve done nothing BUT think about how to do the rehab properly. Maybe it will even help with the zombie and zero energy side effects.
Thanks for your patience. Nobody else listens very well, and with your depth of knowledge. I’m sure I’ll be less needy soon. Newbies are so needy!
LikeLike
I think you might find the online support community at WomenHeart more useful than my blog, Alicia. First of all, they have over 28,000 members in that group, all with heart disease. That’s 28,000 potential listeners. It’s free to join, and “open” 24/7. There’s even a “journal” option in which newbies can write as much as they need to, and a “discussion” option for those who just have a specific question they want to run by other women. This site was a lifesaver for me in the early weeks and months, post-MI.
By comparison, here at Heart Sisters, I’m only one person (and a heart attack survivor also living with the debilitating symptoms of coronary microvascular disease every day) so keeping track of/responding to comments here is harder for me than it would be for the very large group of women members at WomenHeart. Check it out and see what you think…
LikeLike
Thank you so much! I was worried I’m basically whining about stuff as a new patient which I should be addressing elsewhere – and I realize there’s only one of you. I’ve been curtailing many of my comments (probably nothing new in them) for that reason. There is a difference between commenting on a subject and monopolizing – I’ve dealt with it once or twice on my own blog, and that’s a writer’s blog, fairly uninteresting to most people.
Many thanks for the link.
Looking forward to your posts in my feed.
LikeLike
As a 15 year old I was left alone in hospital before and after open heart surgery, visiting was strictly every 2 days during the week and Saturday and Sunday for 1 hour at a time, not like it is today, especially for children, and no one was allowed to see me for 2 days after my op.
I’ve had heart attacks which resulted in cardiac arrests since and a stroke and without a pacemaker fitted, I wouldn’t be here. The worst anxiety I suffered was going home after the heart attacks, feeling very afraid in case it would happen again. I’ve suffered from “panic attacks” most of my life, but no one that I have come across is the least bit interested. I also developed a phobia about going into hospital when I was young, but again no one cared.
As a result I now feel totally alone when I have to have something done, like when I need tests done or a new pacemaker fitted. I say in the past the worst anxiety was after my heart attacks, but I am having tests for heart failure and have in the past week had THE worst anxiety I have ever known. After about 6 months of waiting for results of tests and appointments for more tests, I think it all gets too much and something has got to give. I feel that the mental health of patients who have been through the trauma of heart related illness is largely forgotten but needs to be seriously considered.
LikeLiked by 1 person
Thanks for sharing your unique perspective here, Mag. Those hospital visiting hour schedules sound positively barbaric now, don’t they?! You are so right: the mental health of heart patients does need to be seriously considered. But patients are often the least able to advocate for such consideration during stressful, frightening medical procedures. This sea change in attitude towards supporting a mind-body connection needs to start with care providers and hospital administrators who are the ones who can actually lobby for providing mental health professionals, cardiac social workers, peer support groups and other resources to address that connection. Read more about PTSD in heart patients, and please make an appointment to talk to a counselor, your pastor or a therapist.
LikeLike
I had unexpected lifesaving heart surgery at the age of 48.
Within 6 weeks of my surgery, my mother died (she had terminal cancer and dementia), then when I returned to work, only a few months later, my job contract ended.
Strike 3 and I was out.
People tell me how well I look now. Outwardly yes, but inside I am struggling. Every single day. Nobody sees that.
Please read my blog. I’ve included a few posts about the mental aspects of preparing and recovering from heart surgery.
LikeLiked by 2 people
Strike 3 is one way of describing those three significant and traumatic events, all so close together, but the analogy is limiting (because even when a batter strikes out in baseball, another time at bat is always ahead as the game continues). I spent many years working in hospice palliative care, and your experience reminds me of what we called “complicated grief“. You are not alone. It’s very common to feel “stuck” after multiple losses like yours. When you’re struggling every day, it’s time to seek professional counseling to help yourself. Best of luck to you.
LikeLike
My brain will apologize to my body from time to time. It wasn’t my body’s choice to be born defective, but my brain signed the surgery contract and made the decision. And then it was anaesthetized and safely out of contact with what happened. My body, unbeknownst to my brain, bore the full brunt of its decision. My brain tells my arms to hug my body, while it apologizes. It might sound weird, but I’ve found myself less anxious. Healing hugs to all.
LikeLiked by 1 person
Marie, what a poetic and creative way to view this pervasive conflict between mind and body. Love those healing hugs… Thanks for this!
LikeLike
Oh, Marie, I do that, too. Thanks for sharing. Healing hugs back at you.
LikeLike
The mind/body connection is real and most of us forget that while we are in the throes of recovery from open heart surgery.
I was on a heart-lung machine for 3 1/2 hours while the medical team worked on replacing my aortic valve, then piecing everything that had been separated in my chest back together. For those 3 1/2 hours my brain thought I was dead, as a psychiatrist (who I finally agreed to consult) told me.
When I came out of the anesthesia my brain said, “WTH, I thought you were dead?” What happened? The psychotic events came along with the physical recovery: confusion, delusion, panic attacks, disorientation. For many women, these reactions are part of the recovery process that we are not warned about. These occurrences pile on top of the pain, physical weakness and strong drugs our body had never experienced.
My astute cardiologist told my husband to get me into therapy because the meltdowns were not good for my recovery. I went for a few sessions and once I understood what was going on, the anxiety dissipated. This June, it will be seven years since my surgery. I have many heart sisters locally and around the country. It’s a good feeling to know you are not alone!
Besides my family and friends, excellent medical/mental care and cardio rehab, WomenHeart: The National Coalition of Women with Heart Disease played a major role in my successful recovery.
LikeLiked by 1 person
Astute comments, Ree! Whenever I hear of a patient saying “we were not warned about…” _____ (fill in the blank, anything like the responses you and many other heart patients commonly experience, I wonder why your “astute” cardiologist hadn’t warned you of this common reaction BEFORE you went into the O.R.? As you say, once you can finally get your brain wrapped around what’s going on, the anxiety can dissipate as that mind-body connection catches up, especially once you realize that you are not alone.
I too found that the WomenHeart online patient community was a daily lifesaver for me in the early weeks and months (currently at almost 28,000 members from all over the world!)
LikeLike
“Sending my emotional brain to the back seat” is exactly what I do, only I call it intellectualizing the situation.
Having gone back to school for a new career, I handed in my last paper for my degree in nursing on the 15th of April, had my gallbladder out (in hospital one night), and started my first job as an RN on May 9. I figured that my exhaustion and difficulty feeling like I was part of the group was due to the learning curve and age difference. Other new nurses were young enough to be my children. Nurses my age were old hands and knew one another well. Uh, hello? Maybe I should have taken 4-6 weeks after the surgery and I would have been relaxed and ready to start the job and be sociable, instead of physically struggling myself as well as learning a new job in which I had to keep patients safe and support them when I needed support.
When I had my mitral valve replaced with open heart surgery, I had been sick at home as an “urgent outpatient ” for 15 months. I was married, in my 40s and my mother came from across the country to help. She, in her 70s, was very worried about me, although I was very matter-of-fact about the whole business. There were complications with my recovery so I was in hospital two weeks. When Mum went home, she was still worried, while I was explaining that recovery can be slow.
Not just slow, it turned out. When the home care nurse came, she listened to my lungs and arranged for me to go back to the hospital because there was fluid in one lung. Aha! No wonder walking had been so tiring, there was a good medical explanation. More than a litre was drained from my lung in that week-long stay before I went home and recovery really started.
It took me a long time to realize that while lots of people have mitral valves replaced, I had had more to recover from than I realized. Thirteen years later, two years after my tricuspid valve was also replaced with open heart surgery, I was in CCU with large clots on both artificial valves. I had to lie in bed as still as possible. The cardiac team researched and discussed a treatment plan with me, then used a clot-buster successfully (instead of a third open heart surgery to replace the valves). My discussions were also with the ICU and stroke teams.
About a week after I got home, my legs got shaky and I felt overwhelmed by the realization what a death-defying experience I had just had.
Intellectualizing my situation works for me in the short term. In hindsight I can see it behooves me to take the time and energy after to consider the whole picture in order to achieve my healthiest outcome.
LikeLiked by 1 person
Terrific examples here of ‘just getting on with it’, Jenn. You also mentioned a really interesting story of your Mother coming out to take care of you: she was already anxious about you, so your ‘matter-of-fact’ response to her was likely an attempt to not worry her any further. Women tend to do this (thus protecting those around us) by pasting on that little happy-face smile, despite whatever we may be enduring. I worked with nurses for many years – all of whom said that nurses make the worst patients (for all the reasons you point out for us!) Hope you are enjoying some healthier outcomes these days…
LikeLike
OMG! Are you psychic? This couldn’t be more appropriate.
Going in to have my aortic aneurysm repaired on March 7th. I know I’m very much like the author, putting my emotions in the back seat while I go through rafts of pre-op tests, organize care for when I’m recovering at home, and wrap things up at work. Right now I’m just bewildered that there were no symptoms to alert me about this thing, but I can see where that can turn into anger.
I’m going to keep this blog to refer back to and get help for my head as well as my heart post-op. Thanks Carolyn.
LikeLiked by 1 person
Thanks for weighing in here, Deborah! Delegating your emotions to the ‘back seat’ is simply doing what you know how to do right now. I think even becoming aware in advance that a delayed reponse is common is important, and this foreknowledge will help you, because unlike Summer, you won’t be shocked or surprised when your emotions start climbing back into the front seat. Are you able to come to our talk this Tuesday at the Monterey Centre? I think it would be fabulous if you could attend, especially to hear Dr. Martha Gulati speak before your March 7th procedure.
LikeLike
I was going to go, but now have a pre-op angiogram scheduled for that day. I understand I might be a bit of vegetable as a result. Disappointed!
LikeLiked by 1 person
Best of luck with your angio – hope it all goes uneventfully…
LikeLike
Its only been 5 weeks since my heart attack and my problem is my husband…
He has been a heart patient for 25 years and suffers from venous insufficiency as well. He has been really wonderful until now. Now he has a flareup of gout in his knees so he wants me to go up and down stairs for him and take over waiting on him… I feel like my recovery is suddenly over whether I am ready or not. I look forward to shopping but he has to sit down before me and I cannot finish because I feel rushed…we cannot afford help. There must be some readers who cannot recuperate properly because of a infirm spouse… how do you do it??!!
LikeLiked by 1 person
Hello Chris – I think you’re correct! There must be many people (both men and women) whose recuperation is affected because of the need to be a caregiver. Sometimes a way to get through this is by seeking as much help as you can from outside sources (can you do online shopping/delivery, for example? Can you enlist the help of friends/neighbours/family to keep him company at home while you do the shopping? Don’t make yourself crazy by tackling outings that you know you’re not ready for.
I’m not as worried about you going up and down the stairs for him (that’s good exercise for heart attack patients) but more worried about you feeling stressed or resentful while you’re doing it. I think you may relate to this essay about Dr. Wayne Sotile’s work on family relationships and heart disease.
LikeLike
With me, I coped with heart attack and surgery by believing that they had “fixed” me, so I had no more illness. I went back to work, lived my life and all was well. The following year I fell headlong into unrecognized depression. Then I realized that the disease was still there and would always be.
So, I started doing so many different activities to “prove” I was still a viable person. It finally dawned on me that I was fooling myself to a certain degree. Yes, I am viable, but still sick. But, that is OK. Finally at peace with myself.
LikeLiked by 1 person
Hello Sharen – thanks so much for that very important reminder to all: heart disease is a chronic and progressive diagnosis. Just coming to grips with that reality can be a major shock, and as you describe so well, reality often strikes long after the original diagnosis and treatment. As Summer describes it, her rational brain took the wheel and relegated her emotional brain to the back seat. This reaction is so common that, once again, I wonder why we aren’t warned about this likelihood before hospital discharge… Would mean making peace with it all might be a bit easier!
LikeLike