by Carolyn Thomas ❤️ Heart Sisters (on Blue Sky)
I’ve been sleeping poorly lately. I think I have an ice pick headache coming on. I can’t seem to concentrate. I feel utterly overwhelmed. I cried off and on for an entire day last week. I am clearly distressed.
I recognize this distress because I’ve experienced a similar response in the past – like surviving a misdiagnosed “widow maker” heart attack back in 2008, for example. That was pretty darned distressing. The National Institutes of Health describe distress as “emotional, social, spiritual, or physical pain, or suffering that may cause a person to feel that they are not able to manage or cope with overwhelming changes caused by normal life activities or a serious medical diagnosis.” Those are almost exactly the words I said to a friend just this past week when I was wailing into the phone about my new breast cancer diagnosis: “I just don’t think I am able to get through this!” (You can read more about my breast cancer experiences in these posts).
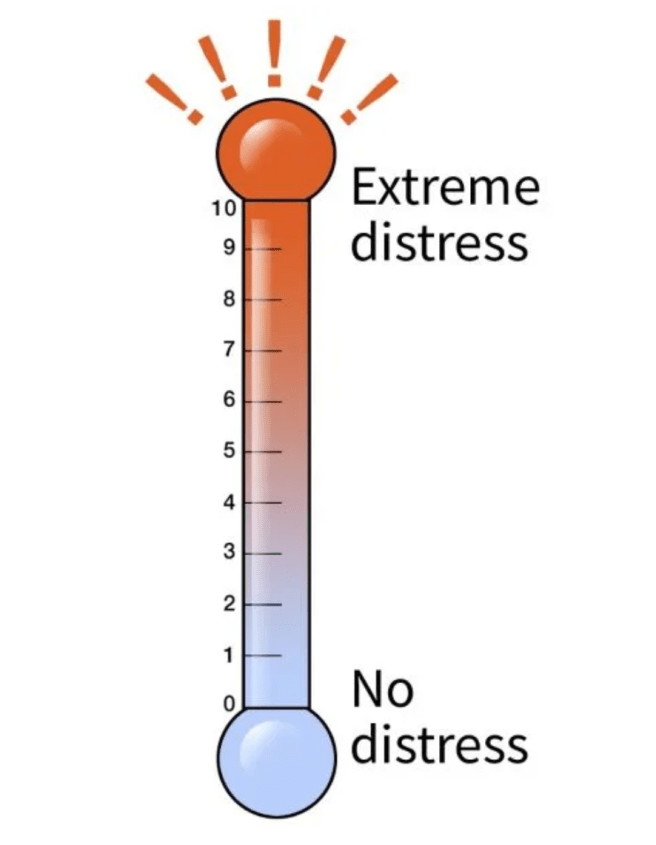
Enter the Distress Thermometer:
Texas researcher Dr. Kristin Ownby explains that back in 1999, the National Comprehensive Cancer Network (NCCN), recommended routine screening for distress in all cancer patients. The Distress Thermometer is used alongside its 32-item problem list of commonly experienced patient issues like fatigue, nausea, lack of sleep, pain, breathing problems, etc.) This was developed as a simple tool to effectively screen cancer patients for symptoms of distress.(1) Dr. Ownby found that, until then, “patient distress was an often overlooked but important reality associated with physical and/or psychological symptoms.”
A 2017 study on distress among cancer patients in America suggested:(2)
- 80 per cent of these patients attribute their distress to financial stressors
- almost 60 per cent have symptoms associated with depression
- 34 per cent report symptoms of anxiety.
Speaking of financial reasons for distress, some of my American friends joke that where I live (here on the beautiful west coast of Canada) it’s some kind of “commie pinko land of socialized medicine”. Consider, for example, that my entire hospital bill for my heart attack hospitalization back in 2008 was zero. Our healthcare system covered the full costs of all of my Emergency Department visits, my diagnostic tests, all cardiac procedures, nursing care, hospital bed, all drugs and treatments during that hospital stay, and annual follow-up consults with a cardiologist.
So imagine my Canadian-style shock recently when our local pharmacy dropped this bombshell on me:
After my new oncologist sent over the prescriptions he’d ordered for chemotherapy treatments starting in two weeks, a pharmacy employee phoned me at home. He advised me that, although the B.C. Cancer Agency fully funds all of my chemotherapy drugs, it will NOT cover the cost of the anti-nausea drugs (for chemo-associated nausea and vomiting due to chemotherapy) or the immune support drugs (to help prevent chemo-associated infections because of lowered white blood cells due to chemotherapy).
And the pharmacy employee then added, in a weirdly casual “oh by the way” tone, that those drugs would cost me $1,100!
I almost had another heart attack, right on the spot.
It wasn’t so much the money that left me gobsmacked (although it did, actually) but it was knowing that somewhere out there is a powerful Cancer Land bureaucrat deliberately deciding that quality-of-life supports like anti-nausea medicine to help vomiting breast cancer patients is not worth funding. That’s a cruel and inhumane decision invented by somebody who I’m guessing has never puked and gagged their way through the chemo appointments which caused the puking and gagging in the first place.
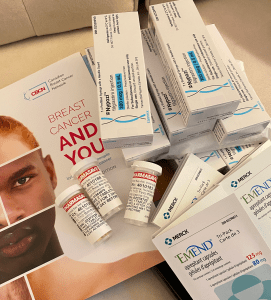
So I phoned our Team Pharmacist at the Cancer Agency (whom I had just met the day before) to help me understand what was going on. And on that same day, she contacted my local pharmacy, and somehow my drug bill magically dropped to “under $100”.
(That’s $1,100 worth of my new drugs on the left)
But for that one awful day, I was clearly able to imagine the dreadful suffering experienced by those 80 per cent of Americans who attribute their patient distress to financial stressors.
Meanwhile, in the Wonderful World of Cardiology, we already know (because heart patients keep telling their cardiologists this) that psychological distress after a cardiac diagnosis is pervasive. This is particularly true among heart patients living with heart failure. See also: my Editorial in the British Medical Journal called “Heart FAILURE: Is it Finally time to Change the F-word?”
Psychological distress that’s ignored is not only absolutely miserable for heart patients to live through, but it’s strongly linked to the inability to follow important preventive recommendations (what physicians prefer to call “non-compliance“) as well as increased hospital re-admissions and worsening patient outcomes.
But when my daughter Larissa and I arrived at the Cancer Agency last week for my first appointment with the breast cancer oncologist, we sat in the lounge and completed a printed survey that we’d been given as soon as we walked in. All of the survey questions asked about how I was coping – emotionally, mentally, and spiritually. This is done routinely in cancer circles. But I’ve never seen a survey like that in all the years I’ve been a heart patient. In cardiology, it seems to be more about bed control: “You’re in a bed. We need that bed. Goodbye and have a nice life!”
Are any cardiology clinics routinely asking their newly diagnosed heart patients questions like the ones listed in the Distress Thermometer to assess the extent of non-physical suffering that we know will impact medical outcomes?
Before I was discharged from hospital after my heart attack, not one person in the CCU (the hospital’s intensive care unit for heart patients) had warned me how predictable mental health distress is among heart patients. Not one doctor, not one nurse, not one janitor had said even one word to me about this very common problem.
The type of distress that occurs so frequently after a serious diagnosis is what mental health professionals often call a stress response or an adjustment disorder. It typically strikes within weeks following a traumatic life event as we struggle to make sense of something that makes no sense. It would help if somebody, anybody told us before hospital discharge that this kind of patient distress is common, predictable and usually temporary. Instead, I felt like I must be losing my mind back then.
Trying to make sense out of something that makes no sense is again what I’m struggling through right now, from the unique lens of a person who has first-hand experience with distress – first in cardiac care and now in cancer care.
I’m thinking I’ve been scoring a solid 8+ on the Distress Thermometer all week. The most obvious difference I’ve noticed between cardiac care and cancer care so far is that I’m automatically offered free support groups and appointments at the Cancer Agency’s Patient & Family Counseling Services. This is the kind of professional help that I had to hunt down and beg for after my heart attack.
And that’s distressing.
♥
1.Ownby K. “Use of the Distress Thermometer in Clinical Practice”. J Adv Pract Oncol. 2019 Mar;10(2):175-179
2. 2) Khera N et al. “Setting the stage for universal financial distress screening in routine cancer care.” Cancer. 2017 Nov 1;123(21):4092-4096.
.
See also: When are Cardiologists Going to Start Talking about Depression?
♥
Q: How are you scoring this week on the Distress Thermometer?
.
NOTE from CAROLYN: My blog-turned-book, A Woman’s Guide to Living with Heart Disease is based on many of my 900+ blog posts about women’s unique experiences with heart disease. You can ask for it at your local library or neighbourhood bookshop (please support your favourite independent bookseller) or order it online (paperback, hardcover or e-book) at Amazon – or order it directly from my publisher, Johns Hopkins University Press (use their code HTWN to save 30% off the list price).

I remember reading somewhere that when we report our pain levels, we should always add our level of distress. I know my pain tolerance is quite high… so what is a 2-3 to me might be a 6 to someone else.
But if I go to the ER perhaps I could say: My pain is a 3 but my distress is an 8 because this came on suddenly and it’s a new symptom.… I like this idea a lot. Especially since the pain scale is so subjective, adding another layer gives professionals an added layer of info.
LikeLike
Hi Carolyn,
I’m so sorry you are having to go through all this. Breast cancer and heart disease are both distressing for sure, and I have experienced the same discrepancy in care between the two.
I was actually shocked to go to a follow-up oncology appt and have 2 nurses asking me in thorough detail (before seeing the doctor) how I was coping in every area of my life, including spiritual. That has never happened to me before in a medical office.
As for the medical bills, I’m sorry you had such a shock. I couldn’t begin to count how much we’ve had to spend on medical bills of all kinds over the years — like my regular diabetes medicine having a retail cost of over $4,703 but thankfully only having to pay $60 out of pocket. Insane!
But worst of all was the bill for my 15 cancer radiation treatments, which were all I needed after surgery — no chemo. Over $57,000 before insurance adjusted and paid — I think it worked out to like $3,500 for each 15-minute session. Fortunately my final cost was a little over $2,200, which I am paying off with a monthly payment plan.
And I’m actually still waiting for the bill for the lumpectomy surgery, which was done last August. I understand the hospital and insurance are in dispute about the bill — insurance is refusing to pay for the surgeon’s assistant, claiming it wasn’t needed to have one?!
I hope your chemo and other treatments go really well and that you don’t get any more surprise bills. Also hoping you can find ways to bring that distress level down!
LikeLike
Hello Meghan – that example you mention of nurses asking a patient how they’re coping “in all areas of life” – well, that’s every patient’s dream scenario. I too have never experienced anything remotely similar in 18 years of being a heart patient.
When I mentioned my shock at that $1,100 bill from my local pharmacy, it’s important to remember that part of the reason I was so shocked is how rarely Canadians (who don’t have to deal with for-profit health insurance companies) ever see that kind of invoice. The average cost for the hospital stay and treatment for an uninsured heart attack patient is over $53,000 BUT even in those with a workplace health insurance plan, my American friends regularly describe insurance claims that are routinely denied by comparison. And last year ProPublica investigators wrote: “In dozens of court cases, judges ruled that health insurance companies had violated federal laws meant to protect people who get health insurance through their jobs…”
Thanks for your kind words. . . Take care. . . ❤️
LikeLike
Heart Failure and Distress
I checked my blood pressure (new Omron cuff) and thought it must be broken when my pressure was better than ever but didn’t understand why my heart rate was at 30! Finally in desperation, I made the call. When I arrived at the ER, they informed me I was in a serious state of Congestive Heart Failure!
Why didn’t anyone realize this before? I didn’t understand. I knew I had put on an excessive amount of weight (it was in my charts) but no one picked up on the fact that it was all the water around my heart. I was in extreme distress! I just assumed that it was just my Lupus as I had been told so damn many times before. So I couldn’t believe what was happening.
I suddenly (?) had a complete blockage? They kept me overnight and at 1:30 the following day (how bad could it be I wondered) and put in a “temporary pacemaker”. The following day again after 1:30 pm, they planned another cath. I was very distressed and angry. I finally had a nurse on ICU come in and lay it on the line about just how severe the situation was! I was ready to give up entirely. After the cath, and another day again after 1:30 pm, I was given a permanent pacemaker. The next day, I was sent home and told not to use my arm for 2 weeks.
After the 2 weeks were over, I began to try and live my normal life again. Two weeks later, I had more tests and saw NP who said my limits were for 4 weeks! Why didn’t the hospital say so?
Anyway, I am now recovering, and the swelling is finally going down. I still feel distressed and angry about all that happened, especially when everyone questions why it took so long for this to be discovered. I have no answers but am glad the worse is over. My poor husband of 53 years is still distressed and worries I will drop dead on him as much as I try to tell him I’m better. We still cannot sleep together and not sure we ever will be able to.
I’m not sure what happened and why no one put the pieces together or recognized that I was in heart failure. But I am happy to be here and finally healing, though I worry about what could happen next. I still have issues with retaining fluids and problems getting that worked out.
I cannot imagine what you are going through, Carolyn, with your new diagnosis. My prayers are with you and I hope you know your readers care about you. Thank you for all your writing over the years, I have enjoyed them immensely.
Love to you and all my heart sisters.
LikeLike
Hello Valerie – first, thanks so much for your kind words about my new diagnosis. I did NOT see this one coming!
I’m sorry you’ve been diagnosed with Congestive Heart Failure (a terrible and hurtful name for a heart condition, by the way!) but happy that you’re healing. I hope you’ve finally “turned the corner” and that every day means you’ll feel a bit better, day by day.
I’ve learned that it’s not uncommon for medical professionals to have totally differing opinions about a patient’s condition – as in your case, was your Nurse Practitioner correct about waiting 4 weeks, or was your pre-discharge hospital instruction (2 weeks) correct? What’s a patient to think? We’re often in such a hurry to feel “normal” once again that it’s common to overdo things. Slow and steady wins the race, right? Yet I’m already wondering how I’ll manage the next 11 months of chemo without going stir crazy…
I’ve come to believe that so much of medicine is simply trying to figure out what the problem is NOT – by ruling out possible issues and discarding the least likely guesses as the test results continue to come in.
I’m not a physician, but I can say that one unfortunate yet credible reason you may feel like you haven’t been thoroughly treated or accurately assessed is that you’re a woman. Lots of good scientific research on this topic – and the frustrating results are simply that gender bias is alive and well in medicine. We live with a healthcare system that has been designed, developed, researched and used on (white, middle-aged) men. As you start to feel better day by day, remember that your only job now is to become the world expert on your new diagnosis! Knowledge is power!
Take care. . . Hope you feel much better soon…❤️
LikeLike
I’m so sorry Carolyn that you are having to deal with all of this!
You have held a strong shield to protect yourself from overwhelming despair. Perhaps having your daughter to support you, your granddaughter to give hope to you, and Canada’s medical system to provide for you, that will all help you cope through whatever is ahead. 🤞
LikeLike
Teri, I often think about what you have written. I appreciate having Larissa and our Everly Rose (age 10, who told me when I was first diagnosed “If your hair falls out, I decided I will shave my head to support you!” What a sweet girl. I highly recommend grandkids – they are wonderful distractions. And my family and friends have been so kind and generous.
And I’ve had the experience just this past week of that overwhelming despair you mention – which was suddenly interrupted by my 4 year old grandson Zack’s arrival – his first bike ride on the new child seat his Daddy attached to the back of his own bike. I could hear Zack (in his brand new Paw Patrol bike helmet!) laughing and squealing with delight a block away as they rode up! 🙂
There IS that overwhelming despair for sure, but then there’s that profound joy, too – especially watching these ‘little people’ in my life.
I wrote more about this odd reality in “Life is Amazing. And then it’s Awful“
LikeLike
Thanks for the reminder that the joys are mixed in with the ‘horror show’. I wish you many delightful moments.
LikeLike
Since 2009 due to divorce, I fell into the category
“80 per cent of these patients attribute their distress to financial stressors”
“almost 60 per cent have symptoms associated with depression, 34 per cent report symptoms of anxiety.”
I have never been able to dig out.
I have been in extreme distress 9-10 for over six years. It’s painful but it does not kill.
LikeLike
Hello Teri – That’s tragic – living at a 9-10 distress score for over six years??! I wonder if you have somehow developed your own self-help survival skills over those years to cope with your extreme distress – and thus avoid that kind of stress from killing you long before now?
Take care of yourself. . .❤️
LikeLike
What is your question? I’m not sure what you are wondering exactly. I’ll try to answer, if I understood your question. Perhaps it’s a rhetorical statement.
LikeLike
Hi again Teri – I think I was curious about your statement about living at a “9-10 distress score” for over six years. It might be true that that kind of high stress over all those years may not necessarily kill you, but it would very likely take a heavy toll on your quality of life – simply because all your stress hormones like cortisol and adrenaline were coursing through your body day after day So I wondered if over those years, you had come up with ways to cope with your extreme distress?
Thanks for asking me to clarify – hope that helps!
❤️
LikeLike
No, I have not come up with ways to cope with the extreme stress that I experience.
LikeLike
So sorry you are experiencing this, Carolyn. I most definitely can relate to your thoughts re the Distress Thermometer.
A few months ago my family doctor noticed my resting heart rate was too high, which resulted in tests, monitors, cardiologist appts., etc. My most recent appt. resulted in my convincing the electrophysiologist to let me have another month before he increased the beta blocker yet again.
Over the past few months, I’ve researched factors affecting heart rate and arrhythmias, (I’m not unfamiliar with this as I’ve had two cardiac ablations) but it wasn’t until I noticed that my sleep has been poor lately that I decided to google sleep and heart rate and I discovered that lack of sleep may influence heart rate, at least according to what I read.
And so yes, here’s where the distress meter comes in – distress resulting from all sorts of factors is of course going to influence my sleep which in turn influences my health which is affecting the distress meter. It kind of seems that distress and sleep are closely related and both factors also impact health – all sorts of conditions– pretty significantly but may often be overlooked by providers.
I have discovered, FWIW, that even though I use blue light filtering glasses, over the past ten days my sleep has improved by my not using screens of any type before bed- I read a book. I do breathing exercises and some mind tricks to help me go back to sleep after I wake up between 2-3 AM. The better sleep has improved the heart rate and arrhythmias for the past 7-10 days and we’ll see if that continues.
Carolyn, I find also that the Calm app helps with distress. But the impact of distress and sleep are real and need to be considered in our healing.
LikeLike
Hello Helen – Poor sleep seems to be a double-edged sword: it hurts our health, and poor health makes it hard for us to get a good night’s sleep!
I too seem to have a built-in alarm clock that wakes me up (WIDE AWAKE!) at 2 a.m. – very close to the same time every time. I too stop using screens before bedtime after a friend delivered a lovely pile of New Yorker magazines which have become my bedtime stories!
Yesterday, I was organizing the big stash of my new cancer meds and noticed the label on one of my immune-support drugs (to be taken before or after a chemo day, I forget which, some require BOTH before and after chemo treatments!) The original drug label instructions said: “Take 2 tablets in the a.m. and 2 tablets at bedtime” but that direction had been edited, so it now reads: “Take 2 tablets in the a.m. and two more no later than 3 pm same day” – the reason for this edit (from the pharmacist) was that the drug is known to cause irritability and insomnia. If I take this at bedtime, I’d likely never get to sleep!
Good luck with your continued good results seeking a healthier night’s sleep!
Take care. . . ❤️
LikeLike
Carolyn, I’m so sorry you’re going through this. Your comparison between the proactive distress screening and support in cancer care versus the apparent void in cardiac care is eye-opening.
It’s frustrating to think of the added burden that lack of support places on patients already navigating serious diagnoses. And that surprise drug bill is just infuriating – it really brings home the systemic issues you’re highlighting.
LikeLike
Thank you Marie for your spot-on perspective. You’re so right – it’s an added burden, during our most vulnerable time when any extra distress is simply overwhelming.
Take care. .. ❤️
LikeLike